 Definition of Joint Mobilization
Definition of Joint Mobilization
- Joint Mobilization is a form of manual therapy whose intention, as its name states, is to increase the mobility of a joint.
- Unfortunately, because of various definitions and different usages of the term by different professions, there is a lot of confusion as to exactly what joint mobilization is.
Joint Mobilization or Mobilisation?
- Joint mobilization is spelled with a “z” in the United States.
- Joint mobilisation is spelled with an “s” in Great Britain, Canada, Australia, and New Zealand.
Grades of Joint Mobilization
- Perhaps the easiest way to define joint mobilization is to divide it into different “grades” of motion.
- I believe that the easiest and most intuitive method is to divide joint mobilization into five different grades, using Roman numerals as designations. Using this naming method, we have the following definitions of joint mobilization grades:
Grade I – any beginning range of motion (small amplitude)
Grade II – full active range of motion (large amplitude)
Grade III – full passive range of motion (large amplitude)
Grade IV – range of motion into joint play (usually nonaxial motion) with slow oscillations (small amplitude)
Grade V – range of motion into joint play (usually nonaxial motion) with a fast thrust (small amplitude)
- Grades IV and V are identical except for the speed of the mobilization (slow oscillations vs. fast thrust).
- Grade V mobilization is often described as a chiropractic manipulation or adjustment, or high-velocity low-amplitude thrust mobilization/manipulation.
 Quick Definition of “Joint Mobilization”
Quick Definition of “Joint Mobilization”
- For a quick and easy definition of joint mobilization, when the term “joint mobilization” is used, it is usually understood to be Grade IV joint mobilization; performed by the therapist with slow oscillations of nonaxial motion at the end of passive range of motion of the joint.
- But as we have seen above, any motion at a joint is technically defined as joint mobilization.
Joint Mobilization vs. Joint Manipulation
- Technically the terms “joint mobilization” and “joint manipulation” are synonymous.
- However, when the term joint manipulation is used, it is usually implied that it is a Grade V fast-thrust mobilization that is being performed. A Grade V mobilization/manipulation is usually described as a chiropractic manipulation or chiropractic adjustment, or a high-velocity low-amplitude thrust mobilization/manipulation.
Who can perform Joint Mobilization?
- Joint mobilization is a form of manual therapy; therefore manual therapists or manual therapy physicians perform it.
- The legal and ethical scope of practice for a manual therapist to perform joint mobilization depends on the type of joint mobilization, and the type of therapist and where the therapist practices.
- Grade V fast-thrust joint mobilization is usually performed by chiropractic and osteopathic physicians, as well as physical therapists (physiotherapists) and occupational therapists. These therapists and physicians can also perform all other Grades of joint mobilization.
 Can Massage Therapists perform Joint Mobilization?
Can Massage Therapists perform Joint Mobilization?
- In the United States, massage therapists and other “bodyworkers” are not legally or ethically allowed to perform Grade V joint mobilization.
- However, Grade IV joint mobilization is legally and ethically allowed to be performed by massage therapists in most states (an estimate is approximately 40 of the 50 states).
- Grade IV joint mobilisation is legally and ethically performed by Registered/Remedial Massage Therapists (a higher designation of massage therapy education and practice) in most states/provinces of Canada (Registered) and Australia (Remedial).
- In some locations, it might be legal for a massage therapist to perform Grade IV joint mobilization but only if the therapist has had advanced continuing education (CE/CPE) training in this technique.
- It is always best to check with your local Government and/or Association bodies to be sure of legal and ethical scope of practice.
Did you know that DCOMT has over 30 video lessons on Joint Mobilization? Join now to get instant access to lessons like:
Thoracic Joint Mobilization with Active Stretching Technique
Prone Sacroiliac Joint Mobilization Force Vectors
Pin and Stretch Lumbar Spine Joint Mobilization with Pelvis Movement
Joint Mobilization is Joint Stretching
- Even though joint mobilization is named separately from joint stretching, joint mobilization is joint stretching.
- In fact, Grade III is essentially regular stretching that most any therapist, trainer, or Pilates or yoga instructor would perform.
- Grades IV and V joint mobilization are essentially pin and stretch technique (see below).
How is Joint Mobilization Performed?
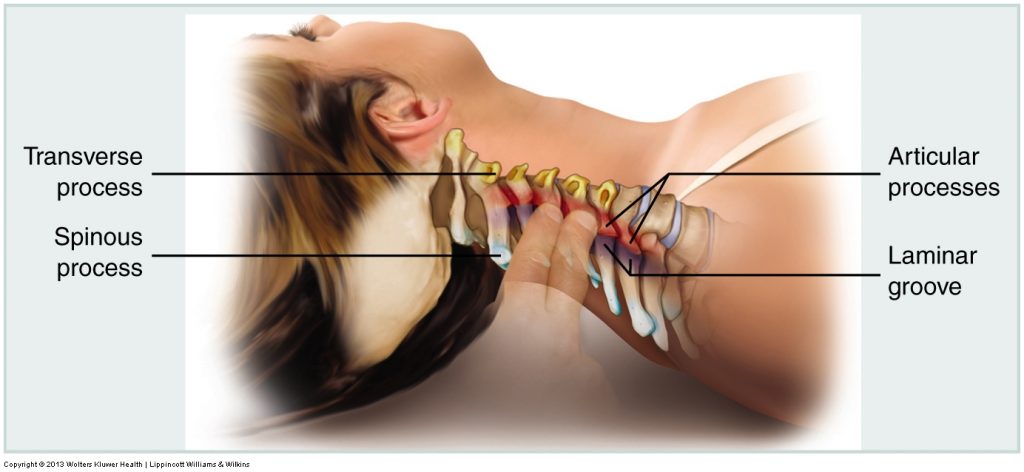
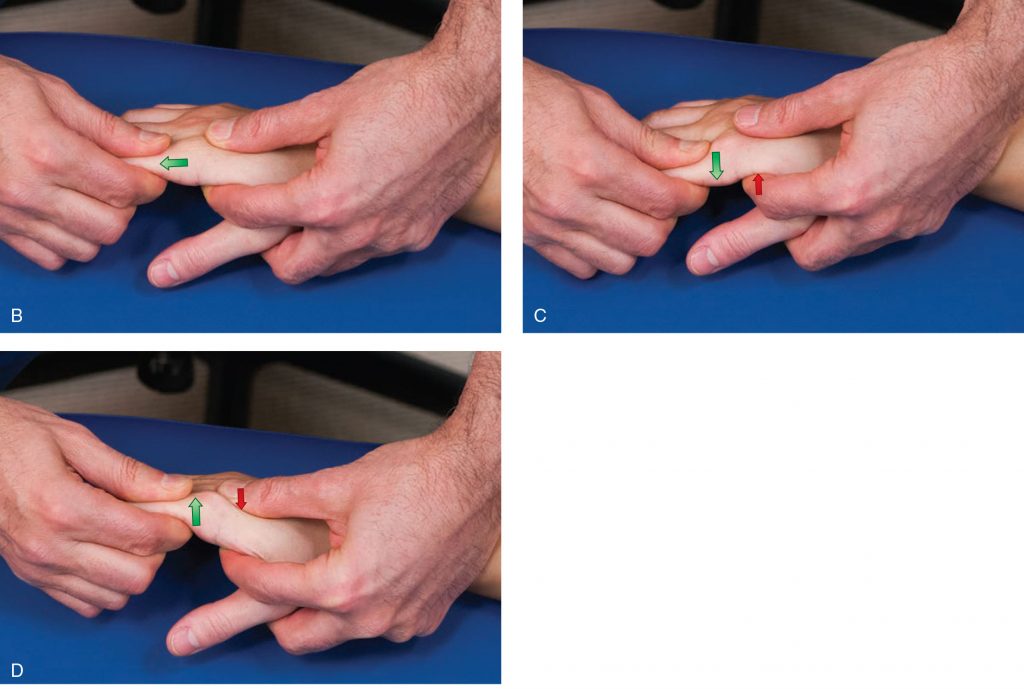
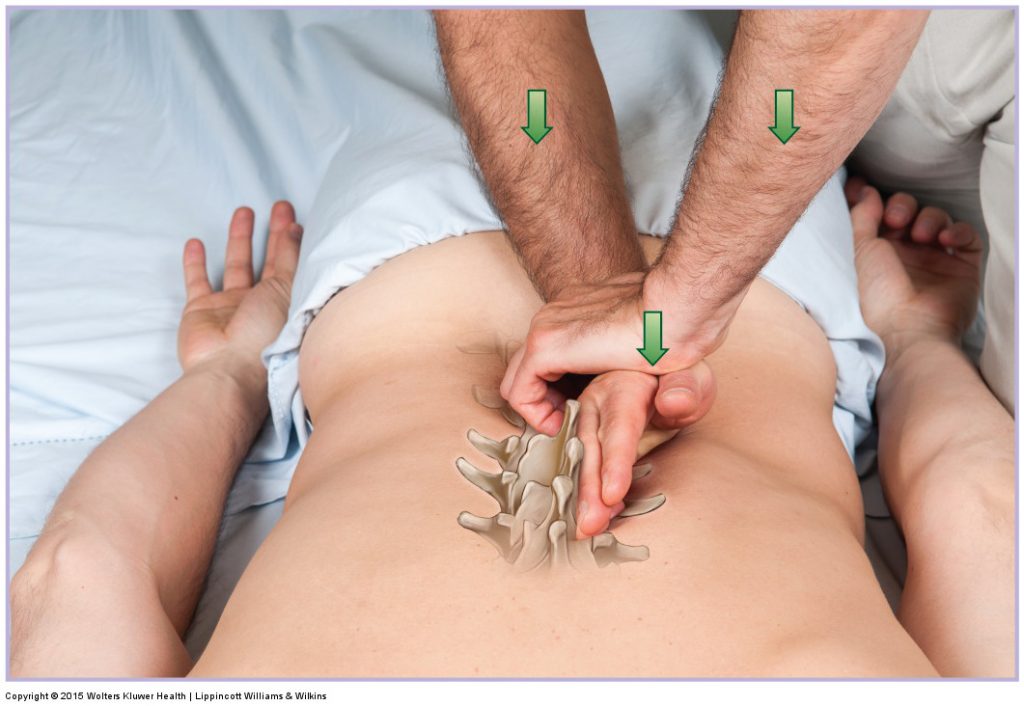
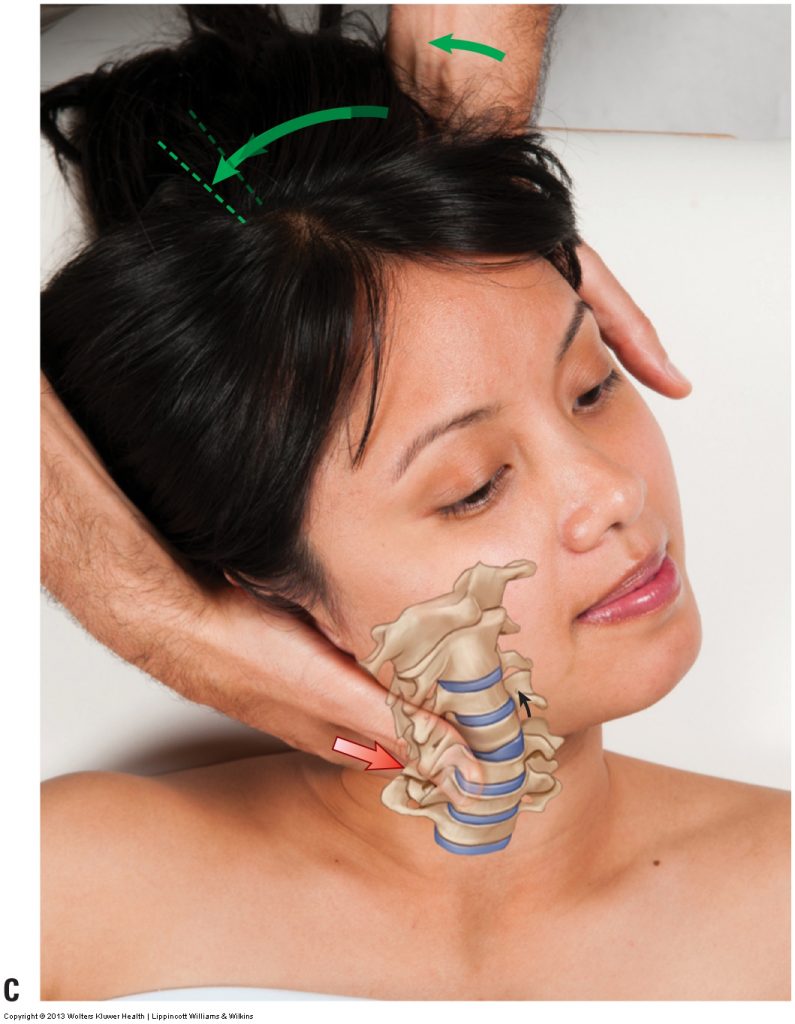
- Grades IV and V joint mobilization are essentially pin and stretch technique.
- Bone “A” is pinned (stabilized) and then Bone “B” is moved relative to Bone “A.”
- The contacts for Grade IV and Grade V must be as close on each bone (“A” and “B”) to the joint surface as possible to achieve nonaxial glide mobilization (if the contact is farther from the joint surface, a regular axial Grade III mobilization will occur instead).
- Therefore, Grade IV (and V) joint mobilization is actually a form of stretching. It is a very specific form of stretching that is aimed at stretching the intrinsic tissue of the joint.
- Joint intrinsic tissue is composed of the fibrous joint capsule, the ligaments of the joint, and intrinsic muscles, if present (for example, rotatores and intertransversarii and interspinales of the spine).
- Grade IV joint mobilization is usually performed with a series of slow oscillations, each movement being very small amplitude, a fraction of an inch/centimeter (literally a millimeter or two) held for a fraction of a second.
- The joint is brought to a tissue tension barrier at the end of passive joint range of motion, and then the joint mobilization force is applied.
- These Grade IV oscillations are usually repeated for a few sets of 3-5 repetitions; or perhaps 10-15 seconds worth of oscillations are performed. As with any form of manual therapy, exactly how the technique is performed is based on the needs and response of the client/patient on the table at that moment.
- With Grade V joint mobilization, one fast thrust is usually performed.
- Mobilizations are repeated for any and all directions of motion that are indicated.
 When should Joint Mobilization be performed during a Manual Therapy Session?
When should Joint Mobilization be performed during a Manual Therapy Session?
- Given that joint mobilization is a type of stretching, as with all stretching, it will probably be most effective if performed after soft tissue manipulation and heat are first done to the area so that the soft tissues of the region will be loose and warmed up, better allowing the joint mobilization to occur.
- Joint mobilization targets stretching the intrinsic tissue of the joint, but the extrinsic (extra-articular/periarticular) soft tissues must be flexible enough to allow the joint mobilization motion, so they should first be warmed up.
What is the Sound When a Chiropractor Adjusts Your Spine?
- During a Grade V fast-thrust mobilization/manipulation, a “popping” (often called “cracking”) sound is often heard. This can be termed “cavitation of the joint” or a “joint release.”
- Contrary to what many people think, this is not the sound of one bone cracking against the other. Rather, it is opposite; it is the sound of the joint opening up.
- In (synovial) joints, there is fluid fully enclosed within the joint capsule. During the mobilization, one bone is stretched away from the other bone, increasing the volume in the joint, which thereby decreases the pressure within the capsule. To equalize this decreased pressure, gases dissolved in the synovial joint fluid come out of solution, creating the popping sound.
- This is analogous to opening up a bottle of sparkling wine (e.g., Champagne). When the cork is removed, the pressure decreases and the gases come out of solution making the characteristic sound of “popping open a bottle of Champagne.” If you put the cork right back in and immediately remove it again, there will be no popping sound. But if you put it back in and wait a period of time (perhaps an hour or more), and then remove it again, because the gases had time to go back into solution, the popping sound will occur again.
- It is the same with our joints. If you “pop” a joint, perhaps your finger joint (knuckle/ metacarpophalangeal or interphalangeal joints), you will get a popping sound. Try to immediately repeat this motion and there will be no popping sound. But wait a little while and then repeat this motion and you will hear the popping sound again. As with the Champagne, the joint needs time for the gases to return into solution.
- The popping sound is not important in and of itself. What is important is that the intrinsic tissues of the joint (fibrous joint capsule and ligaments, and perhaps intrinsic muscles if present) are stretched. Remember, this is a joint mobilization and mobilization occurs when soft tissues are stretched to allow motion! The popping sound is simply confirmation that there was a sudden pressure change, indicating successful stretching of the intrinsic tissues.
- The reason that the fast thrust method of joint mobilization is so effective is that it creates a greater force than a slow motion so that it overcomes the coefficient of friction to move the surfaces; and because it is so quick, there is no chance for a muscle spindle stretch reflex to occur, which would otherwise result in tightening up of the muscles, which would then stop the stretch of the mobilization.
- As with manual therapy technique, there are always indications, precautions and contraindications (see below).
Indications for Joint Mobilization
- There is essentially only one indication for joint mobilization: that is a hypomobile joint dysfunction.
- Given that joint mobilization mobilizes a joint, it would only be necessary if the joint has lost mobility, in other words is hypomobile.
- A hypomobile joint dysfunction is often described in static terms of being a subluxation, misalignment, or bone out of place. Usually, mobility loss and static malposition correlate with each other. But ultimately, the decision to indicate joint mobilization is loss of joint mobility.
- To determine if joint mobilization is appropriate for any specific musculoskeletal (neuro-myo-fascio-skeletal) pathologic condition, we need to understand and look at the “pathomechanics” of the condition. If there is joint hypomobility involved, then joint mobilization is indicated.
Precautions and Contraindications for Joint Mobilization
- There is essentially only one precaution/contraindication for joint mobilization; that is a hypermobile joint dysfunction or other unstable tissue.
- Given that joint mobilization mobilizes a joint, in other words increases its motion, then if the joint is already hypermobile, in other words unstable, then it would be contraindicated (or at least precautioned) to mobilize it further.
- Given that mobilizing a joint requires placing a physical force into the body, which affects other adjacent tissues of the body, any tissue instability in the region would contraindicate (or at least precaution) performing the mobilization treatment. For example, a client/patient with osteoporosis or a herniated disc may not tolerate the physical force necessary to perform the mobilization technique.
- Because Grade V mobilizations generate the most force, precautions and contraindications are greater for them.
Fuller Understanding of Joint Mobilization…
To better/fully understand joint mobilization, let’s define a few terms…
 Range of Motion (ROM)
Range of Motion (ROM)
- The term range of motion (ROM) means exactly that; it is the range of motion at a joint. In other words, how far one bone at a joint can move relative to the other bone at that joint.
- Depending on the joint, there may be varying RsOM possible. For example, a triaxial joint like the glenohumeral (shoulder) joint, would have more RsOM than the elbow joint, which is a uniaxial joint.
- RsOM are usually named for cardinal plane (sagittal, frontal, transverse) component motions. So the elbow joint can move into flexion and extension in the sagittal plane; whereas the glenohumeral joint can move into flexion and extension in the sagittal plane, abduction and adduction in the frontal plane, and lateral (external) rotation and medial (internal) rotation in the transverse plane.
- Certainly, we could also describe oblique plane ranges of motion as well.
- So when a range of motion of a joint is described, the direction (e.g., flexion, lateral rotation) of that range of motion is also stated.
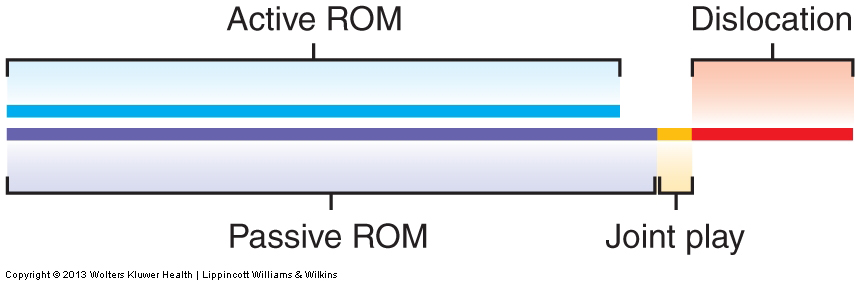
Active Range of Motion (AROM):
- Active Range of Motion (AROM) is defined as the ROM that a joint can move when moved by the contraction of the musculature of that joint.
Passive Range of Motion (PROM)
- Passive Range of Motion (PROM) is defined as the ROM that a joint can move when moved by a force other than the musculature of that joint.
- A therapist could provide this other force.
- But this other force could also be provided by the client himself/herself; for example, one could use their right hand/arm to move the neck into a range of motion.
- PROM is generally slightly greater than AROM.
Joint Play
- Joint Play is defined as the small amount of nonaxial glide that is possible at a joint at the end of PROM.
- Beyond joint play is dislocation.
- Motion in joint play is usually nonaxial.
Axial vs. Nonaxial Motion
- Axial motion occurs around an axis; nonaxial motion does not (see below for more detail).
Axial Motion
- An axial motion is a motion in which one bone moves around an axis.
- An axis is an imaginary line, usually passing through the center of the joint, around which motion occurs.
- Because the motion is “around” the axis, the motion is circular.
- Axial motions are also known as circular or angular motions.
- Most joint motions that therapists think of are axial; for example flexion, adduction, right rotation, to name a few. With an axial motion, different points along the bone that is moving would move different amounts.
- Points closer to the axis (i.e., the joint) transcribe a smaller circle than points that are farther from the axis.
- An analogy could be made to an old-fashioned vinyl record player. A point closer to the center of the record spins around the axis/center and transcribes a smaller circle than a point closer to the periphery of the record.
Nonaxial Motion
- A nonaxial motion is a motion in which the bone does not move around an axis.
- Therefore each and every point on the bone that is moving would move the exact same amount.
- Nonaxial motions are also known as gliding, sliding, or planar motions.
 Fundamental Components of Motion
Fundamental Components of Motion
- Even though most therapists learn terms of motion such as flexion and abduction, there are actually fundamental motions that underlie these more familiarly named motions.
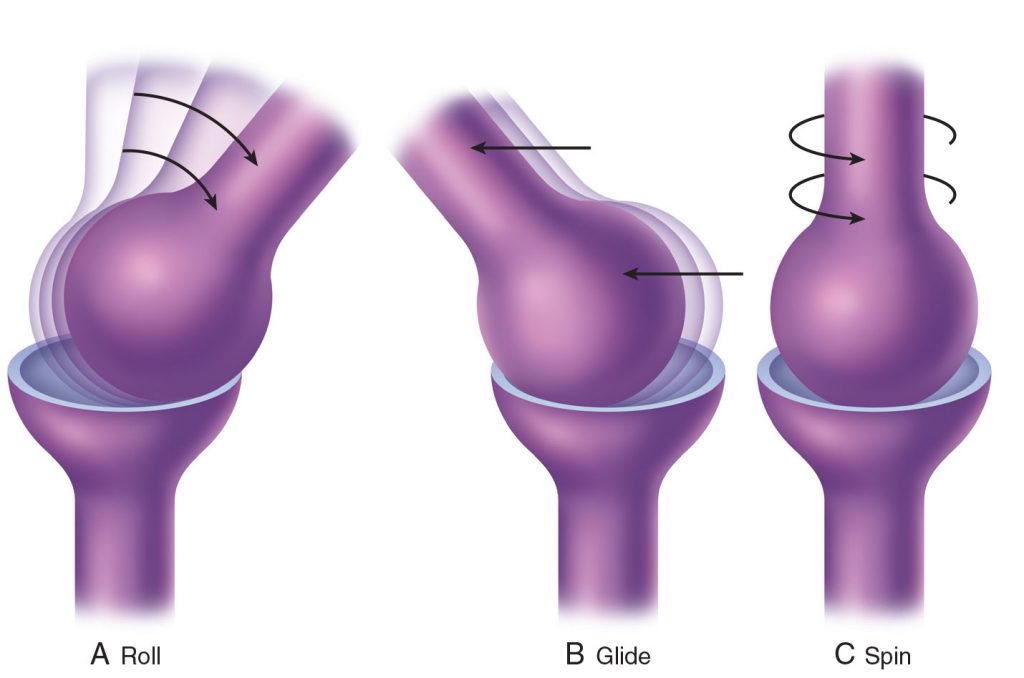
- The three fundamental types of motion that underlie all motions are spin, roll, and glide.
Spin
- Spin is a pure rotation, usually a long-axis rotation, in which one bone spins upon the other bone around the long axis of the joint.
Roll and Glide
- Roll and glide are usually considered together because when roll occurs, it must be accompanied by glide for healthy joint motion to occur.
- Roll is an axial motion; glide is a nonaxial motion.
- Essentially, when the articular surface of one bone rolls on the articular surface of the other bone, it would roll “off” the other bone (in other words, dislocate) if there were not some compensatory glide.
- Even if one bone were to not roll all the way “off” the other bone, if it did a pure roll motion, it would no longer be centered on the articular surface of the other bone.
- The term “centration” describes the optimal positioning of one bone being centered on the other. This is optimal because the articular cartilage is usually thickest at the center of the articular surfaces. Articular cartilage is necessary to cushion the compression forces of the two bones against each other.
- There are two types of compensatory glide that accompany a roll motion.
- When a convex bone moves on a concave one (termed convex on concave kinematics), the glide is in the opposite direction of the roll. An example would be the head of the humerus (convex) moving along the glenoid fossa of the scapula (concave).
- When a concave bone moves on a convex one (termed concave on convex kinematics), the glide is in the same direction as the roll. An example would be the proximal end (base) of the proximal phalanx (concave) moving along the distal end (head) of the metacarpal at a metacarpophalangeal joint (convex).
- Understanding how the nonaxial glide relates to the axial roll at a joint indicates how the joint mobilization should be applied. For example, at the metacarpophalangeal joint, if there is a loss of axial extension of the finger, then because finger extension involves a dorsal roll with a dorsal glide (concave on convex kinematics), then the nonaxial glide mobilization that would be needed would be dorsal glide.
How is Joint Mobilization Assessed?
- Joint mobilization is a manual therapy treatment technique.
- The manual therapy assessment technique can be called motion palpation.
- Motion palpation assessment technique and joint mobilization treatment technique are identical to each other. The only difference is the intent.
- The intent of assessment is to assess/diagnose, in other words, determine the integrity/health of the joint motion. In other words, does the joint have full and pain-free range of motion?
- The intent of treatment to treat, in other words to improve the integrity/health of the joint motion.
- When motion palpation assessment is performed, both the degree of range of motion as well as the “end-feel” of the joint motion is assessed.
- A hypomobile joint usually has a “hard end feel.”
- A hypermobile joint usually has a “mushy end feel.”
- A healthy joint usually has a “firm but slightly springy end feel.”
Where Can I Learn Joint Mobilization?
Dr. Joe Muscolino‘s The Art and Science of Kinesiology has various levels of Certification in Clinical Orthopedic Manual Therapy (COMT), including joint mobilization technique. These levels are:
- COMT Intensive Certification (Level 1)
- COMT Intensive Skillset Certification (Level 1)
- COMT Master Class Series Certification (Level 2)
- Digital COMT is a video streaming subscription service that covers all manual and movement techniques, including joint mobilization.


