Introduction to Musculoskeletal Pathologies of the Low Back and Pelvis
 Note: This blog post article is the first in a series of twelve articles on musculoskeletal conditions of the low back (lumbar spine) and pelvis. For the rest of the articles in the series, scroll to the end of this article.
Note: This blog post article is the first in a series of twelve articles on musculoskeletal conditions of the low back (lumbar spine) and pelvis. For the rest of the articles in the series, scroll to the end of this article.
Proper therapeutic treatment of a client’s/patient’s low back and pelvis depends on an accurate assessment of the client’s condition(s) as well as a clear understanding of the mechanism of the pathologic condition(s) that the client is experiencing.
Each pathologic condition has a unique physiologic mechanism, pathophysiology or pathomechanism, that, when understood, can guide critical reasoning regarding the therapeutic tools that should be used. Rather than asking the learner to apply a memorized “cookbook” routine from one technique or another that may be ineffective or perhaps even hurt the client, this blog post article will encourage learning how to choose the technique protocols that will safely and most effectively help the client.
Note: This blog post article is the first in a series of twelve articles on musculoskeletal conditions of the low back (lumbar spine) and pelvis. For the rest of the articles in the series, scroll to the end of this article.
Hypertonic / Tight Muscles of the Low Back and Pelvis
Hypertonic, or tight muscles is an important condition to discuss for two reasons:
- It is the most common presenting complaint that a manual therapist will confront.
- It is usually a component of every other musculoskeletal condition of the low back and pelvis.
Of further significance is the fact that tight muscles are so often ignored by conventional medical professions. There are medical specialties for every organ system of the body, but there is no “muscle doctor.” Even the chiropractic profession usually relegates the importance of tight musculature to a position of lesser importance compared with joint positioning and function. Perhaps the importance of tight musculature is overlooked because it does not show on x-rays, other radiographic imaging, or in laboratory results. For this reason, manual therapists who are highly trained in muscle palpation assessment skills and soft tissue treatment techniques have the opportunity to step into this niche.
Description of Hypertonic Musculature (tight muscles)
A hypertonic muscle is one that has too much tone; “hyper” denotes an excessive amount. Tone refers to tension; in other words, it is the pulling force of a muscle. The degree of tone that a muscle has varies based on the degree of its contraction. There are two types of hypertonic musculature: a globally tight muscle and a myofascial trigger point (TrP). The first term is used to describe an entire muscle or large portion of a muscle that is too tight; the second term is used to describe a small focal area of muscle tightness that can refer pain to a distant site.
(Note: This article will address globally tight musculature. Myofascial trigger points will be addressed in the next blog post article in this series.)
Globally Tight Musculature
When you consciously contract a muscle, its tone is high. However, when a muscle is at rest and you are not consciously directing it to contract, other than a small amount of baseline tone to maintain the posture of the joint, it should be relaxed. This condition is called resting tone. A resting tone greater than the amount needed to maintain joint posture is what defines a muscle as being hypertonic. Other terms often used synonymously are spasm, cramp, and contracture, all of which essentially describe a muscle whose baseline tone is excessive or hypertonic.
Mechanism of Globally Tight Musculature
The physiologic mechanism of a globally tight muscle is determined by muscle spindle fibers (also known as intrafusal fibers or spindle cells). Muscle spindle fibers are located within the belly of a muscle and lie parallel to the regular fibers of the muscle. Similar to these regular muscle fibers, spindle fibers have the ability to contract and relax. But they also possess another feature that regular muscle fibers do not. Muscle spindles are receptor cells that have the ability to detect when they are being stretched. They are sensitive to both how quickly and how far they are stretched. The sensitivity of their setting is determined by the gamma motor system of the brain, which can order them to contract and tighten or allow them to be relaxed and loose. The tighter the muscle spindles are set, the more sensitive they are to stretch; the looser they are, the more tolerant they are to being stretched.
If a muscle is stretched, all of the fibers within the muscle, both regular and spindle, are lengthened. If this stretch occurs quickly or is farther than the spindle fibers can comfortably allow, it sends a signal via a sensory neuron into the spinal cord. This sensory neuron then synapses with lower motor neurons (LMNs) that return to the muscle, ordering the regular fibers of the muscle to contract (Fig. 1). This is called the muscle spindle reflex, or stretch reflex (or myotatic reflex), and is protective in nature. By tightening the muscle, the stretch is stopped, and the muscle is protected from being overstretched and perhaps torn.
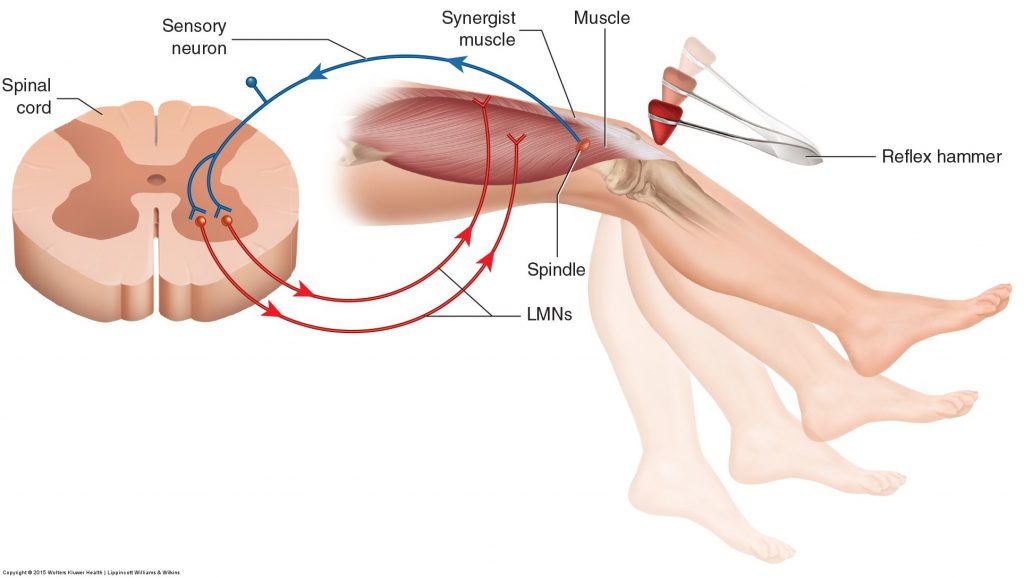
Figure 1. Muscle spindle reflex. A reflex hammer is used to strike and cause a quick stretch of the distal tendon of the quadriceps femoris (knee joint extensor musculature), triggering the muscle spindle reflex. A signal is sent to the spinal cord via a sensory neuron. In response, a signal is sent from the spinal cord through lower motor neurons (LMNs) to tell the muscle to contract, causing extension of the leg at the knee joint. Permission Joseph E. Muscolino. Manual Therapy for the Low Back and Pelvis – A Clinical Orthopedic Approach. 2015.
The stretch reflex is usually only thought of as protecting a muscle from strong forces such as whiplash accidents. However, the stretch reflex is also responsible for setting resting tone of the musculature. When the gamma motor nervous system directs the spindle fibers within a muscle to contract, they shorten. Then when the person moves, as soon as that muscle is stretched even a small amount more than the length of its spindles, the stretch reflex will cause the muscle’s fibers to contract to the tension level set for the spindles. In this manner, the length of a muscle’s fibers, or its tone, will match the length and tone set for its spindles. The term muscle memory is often used to describe this baseline tone of a muscle. Muscle memory resides in the nervous system, not in the muscle itself.
(Click here for a blog post article on Piriformis Syndrome.)
(Click here for a blog post article on quadratus femoris muscle.)
(Click here for a blog post article on psoas major stabilization of the spine.)
Causes of Globally Tight Musculature
There are a number of causes for globally tight musculature (tight muscles). Four of the most common causes are as follows:
- Overuse
- Splinting
- Adaptive shortening
- Overstretching
In each case, the muscle memory tone set by the gamma motor system and the muscle’s stretch reflex is increased. Although this article addresses each cause separately, when a client presents clinically with tight musculature, the mechanisms of the causes can and often do overlap.
1. Muscle Overuse
Overuse of a muscle fatigues it. Overuse also increases its level of tension. This increases the muscle’s pulling force on its tendons and bony attachments, irritating these structures and causing pain. In response to this pain, the nervous system signals the muscle to contract, which creates increased tightness of the entire muscle. This is a protective mechanism meant to decrease or prevent motion that might further irritate or injure the musculature and/or other soft tissues. Muscle tightness causing pain, which then triggers further tightness, which then triggers further pain, and so forth, is known as the pain-spasm-pain cycle. Prolonged contraction of a muscle can also result in a disruption of the blood circulation to the area. Initially, the prolonged contraction interrupts venous return of blood, causing a buildup of waste products. These waste products are acidic and irritate the muscle tissue, causing increased pain, which then further perpetuates the pain-spasm-pain cycle. The result is increased reflexive spasm of the muscle (Fig. 2).
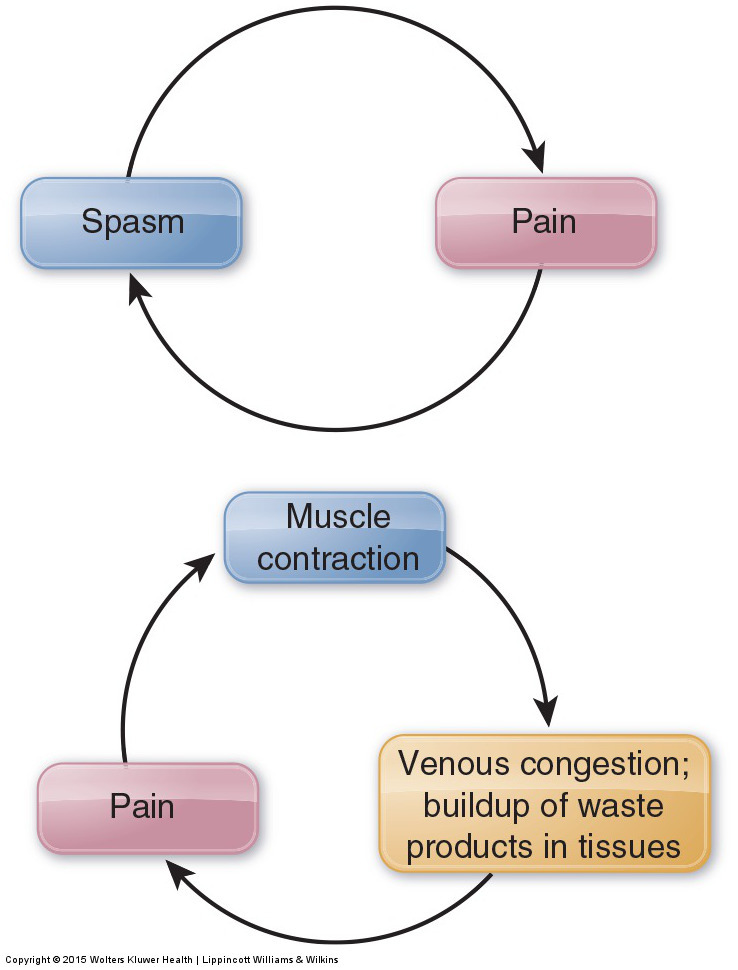
Figure 2. Pain-spasm-pain cycle. (A) A tight (spasmed) muscle pulls excessively on its attachments, causing pain. In response to the pain, the muscle’s tension level increases. (B) When a muscle is tight, its contraction can also reduce venous blood flow, resulting in a buildup of acidic waste products in the area. This causes further pain, which perpetuates the pain-spasm-pain cycle. Permission Joseph E. Muscolino. Manual Therapy for the Low Back and Pelvis – A Clinical Orthopedic Approach. 2015.
Muscle overuse is often thought of in terms of an activity such as playing sports or working out at a gym. If the same muscle or muscle group is used repeatedly without rest, it will gradually fatigue and become painful. However, overuse can also result from prolonged unhealthy postures. Although less dramatic, poor posture is often a greater contributor to muscle tightness than overuse from activity.
One of the most common postures that causes tight muscles of the low back is when the trunk is flexed forward such that its weight is no longer centered over the pelvis. This happens every time that you lean forward to work down low in front of yourself, or when you bend forward to pick up something from the ground. Without muscles to counteract the force of gravity, the trunk would naturally fall forward. Low back extensor muscles, such as the erector spinae, must eccentrically contract to slow your body’s descent as you flex forward, then isometrically contract if you hold the imbalanced forward-flexed posture, and then concentrically contract to extend back to anatomic position (Fig. 3). Because of the tremendous amount of time that many people spend in forward-flexed postures, tightness of the posterior low back musculature is very common.


Figure 3. Prolonged postures and low back tightness. (A) Flexing the trunk when working down in front of the body causes the body weight of the trunk to be imbalanced. This requires isometric contraction of the posterior low back extensor muscles to hold the trunk in this posture. (B) Carrying a baby on a hip requires isometric muscular contraction of the elevators of the pelvis on that side. (Permission Joseph E. Muscolino. Manual Therapy for the Low Back and Pelvis – A Clinical Orthopedic Approach. 2015.)
If the client is pregnant or if the client is overweight with a large abdomen, the increased weight carried anteriorly can imbalance the client’s center of weight anteriorly, increasing the forward flexion force upon the client’s trunk. This would have to be counteracted by the postural isometric contraction of the low back extensor musculature. With excessive work, postural muscles of the low back will likely fatigue and tighten.
Note: Fascial Adhesions
When muscles are tight, another factor that must be considered is fascial adhesions. Fascial adhesions, also known as scar tissue adhesions (or fibrous adhesions, or more simply adhesions), are composed of fibrous fascia collagen fibers (see accompanying figure). These collagen fibers are the same substance that makes up tendons, ligaments, and other fibrous fascial tissues. Although adhesions are normally thought to be deposited in sites of trauma (i.e., scar tissue), they are in fact deposited continuously between the soft tissues of the body. These fibers increase the stability of the tissues by binding/connecting the tissues together. However, if adhesions build up excessively, they may bind together the two opposing surfaces of a soft tissue interface, which should slide along one another when movement is needed; this results in restricted mobility. In a client with an active lifestyle, these fibers do not get the chance to build up because as the client’s body moves, adhesions that have formed are broken up and resorbed. However, a sedentary lifestyle encourages adhesions to build up progressively until mobility is greatly restricted. Although adhesions do not actually cause an increase in the baseline resting tone contraction level of a muscle, they do add to the muscle’s tightness by decreasing the muscles’ ability to stretch and lengthen. If a muscle cannot lengthen, then it cannot allow movements of the body performed by the antagonists to that muscle.
The mobility of ligaments, joint capsules, and all other soft tissue can be affected by adhesions as well. Manual treatment techniques such as massage, stretching, and hydrotherapy all help to break up adhesions in muscles and other soft tissues.
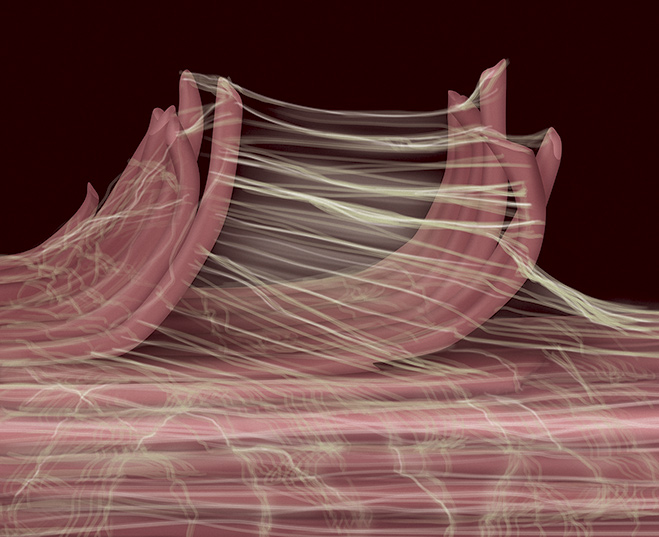
Fascial Adhesion Figure. Fascial collagen fibers have a spiderweb appearance. Educator and author, Gil Hedley, uses the term fuzz to describe fibrous fascia. (Figure permission of Joseph E. Muscolino. Art work by Giovanni Rimasti. Modeled from a photo by Ronald A. Thompson.)
2. Muscle Splinting
Tight muscles of the low back and pelvis may be present not only if the muscles themselves are irritated and overused but also if any other tissues of the region become irritated or injured.
This is especially true of the tissues of the sacroiliac joints and the facet joint capsules and ligaments of the lumbar spine. This phenomenon is called muscle splinting, and it is a protective mechanism for these fragile and vulnerable tissues. By tightening, the musculature acts as a splint to the area, blocking motion and thereby allowing the tissues of the area to rest and heal. Therefore, overt traumatic injury or irritation to any tissues of the joints of the low back and pelvis can cause the muscles of the region to tighten and splint the area.
3. Adaptive Shortening
Adaptive shortening occurs when a muscle is held in a shortened state for a prolonged time and adapts to that shortened state by increasing its tone. Adaptive shortening is a protective mechanism. If a muscle is shortened and slackened, then when it contracts to move the body, the muscle would be unable to generate tension on its attachments until all the slack has been removed. This would not only cause an inefficient delay in movement but it could also be dangerous in a fight-or-flight scenario. For this reason, the nervous system adaptively shortens the muscle by increasing its tone to match the shortened length. The net result is that if a certain posture is held for a long time, the musculature will shorten and adapt to that posture so it is ready to create tension and movement immediately if needed. One example of this is the posture of the hip joint when sitting. Sitting places the hip joint into flexion, shortening the hip flexor muscles that cross the joint anteriorly, attaching from the pelvis to the thigh. This chronic posture of allowing the hip joint to be flexed can result in adaptive shortening of the hip flexor musculature bilaterally. Their tightness will then tend to create an excessively anteriorly tilted pelvis because hip flexor musculature’s reverse action is anterior tilt of the pelvis at the hip joint (see Lower Crossed Syndrome blog post).
4. Muscle Overstretching
Another common cause of tight muscles of the low back is when muscles are overstretched. As described previously, if the low back is stretched too fast or too far, it can activate the muscle spindle’s stretch reflex and cause a spasm. Even though this reflex is protective, the spasming often persists long after the initial event that triggered it, resulting in a chronic posture of tight musculature of the region.
Overstretching a muscle can be caused traumatically, as with a fall or other injury. It can also occur when doing stretches as part of a health and fitness regimen. This is especially true if stretching is done too vigorously when the muscles have not yet warmed up, as often occurs when stretching is done before an exercise routine. For this reason, it is increasingly recommended that stretching be done after exercising, when the muscle tissues are warm. Thus, even though stretching is a valuable part of a health and fitness regimen, when it is performed too aggressively, it can be detrimental to musculoskeletal health. Moderation is the key.
Overstretching also often occurs in a much more insidious and seemingly innocuous manner. Simple postures assumed and carried out during the day can be the culprit. Examples include poor ergonomics at the workplace, such as bending down to work low in front of your body instead of working up higher in front of yourself, or twisting to one side to work off to the side in front of yourself instead of working directly in front of yourself. Postures and activities outside of work can also contribute. Bending forward during hobbies or activities such as cleaning or gardening can overstretch the low back extensors of the spine. Sleep posture can be equally problematic. If the client sleeps in a position that is halfway between side-lying and being on the stomach, the lumbar spine is torqued/rotated. This posture can easily cause an overstretch of the opposing rotator musculature that is antagonistic to this position, resulting in waking during the night or the next morning with tight muscles caused by the stretch reflex.
(Note: Click here for a blog post article on hypertonic tight musculature of the neck.)
This blog post article is the first in a series of twelve articles on musculoskeletal conditions of the low back (lumbar spine) and pelvis.
The articles in this series are:
- Hypertonic / tight muscles
- Myofascial trigger points
- Joint dysfunction
- Sprains and strains
- Sacroiliac joint injury
- Pathologic disc conditions and sciatica
- Piriformis syndrome
- Degenerative joint disease (DJD)
- Scoliosis
- Lower crossed syndrome
- Facet syndrome
- Spondylolisthesis


