This blog post article is part of a series of articles on assessment of the low back and pelvis. Scroll to the end of this article to see the others in this series.
Brief Review of Assessment and Treatment
The following is a brief overview that links the low back condition with its corresponding assessment procedure and its corresponding treatment.
Hypertonic Musculature
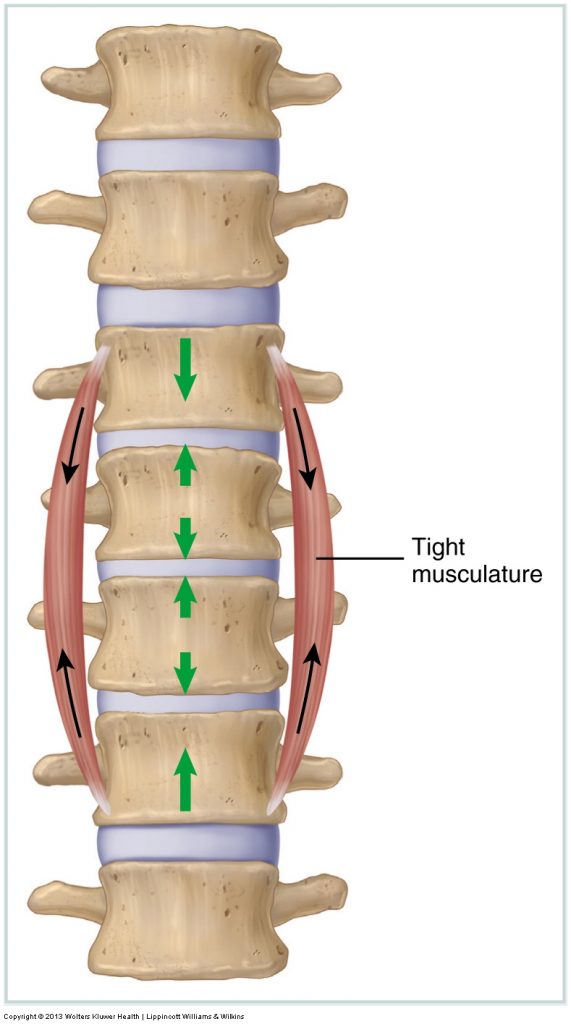 Tight muscles in the low back are assessed by measuring the client’s passive ranges of motion (ROMs). If an ROM is restricted, then the antagonistic muscles (generally located on the other side of the joint) to that motion are most likely tight. Tight musculature is not the only tissue that can restrict joint motion. Whenever an active or passive ROM is restricted, any taut tissues on the other side of the joint may contribute to the restriction in motion, including ligaments and joint capsules.
Tight muscles in the low back are assessed by measuring the client’s passive ranges of motion (ROMs). If an ROM is restricted, then the antagonistic muscles (generally located on the other side of the joint) to that motion are most likely tight. Tight musculature is not the only tissue that can restrict joint motion. Whenever an active or passive ROM is restricted, any taut tissues on the other side of the joint may contribute to the restriction in motion, including ligaments and joint capsules.
Whether they are a result of increased active muscle tone or adhesions, the treatment options available to the manual therapist to help loosen tight musculature and other soft tissues are many, ranging from soft tissue manipulation, to hydrotherapy, and to stretching techniques and joint mobilization.
(Click here for a blog post article on hypertonic / tight muscles of the low back and pelvis.)
(Click here for a blog post article on myofascial trigger points / muscle knots.)
Joint Dysfunction
 Joint dysfunction in the low back is assessed with motion palpation assessment, also known as joint play assessment.
Joint dysfunction in the low back is assessed with motion palpation assessment, also known as joint play assessment.
If a specific segmental vertebral level is found to be hypomobile, then the only effective treatment option is to perform joint mobilization technique. If a client has a hypermobility, a manual therapist can do little to nothing to directly help because every treatment tool that a manual therapist employs is aimed at increasing, not decreasing, mobility. However, if the joint hypermobility exists as a compensation for an adjacent hypomobility, then the hypermobility may be alleviated if the adjacent hypomobility is mobilized. Note: Strengthening musculature around a hypermobile joint is helpful. If strength training is within your scope of practice/license, then it should be employed.
(Click here for a blog post article on lumbar spine joint dysfunction.)
Lumbar Sprains and Strains
Permission Joseph E. Muscolino DC
Manual Therapy for the Low Back and Pelvis – A Clinical Orthopedic Approach (2015)
Assessing a sprain or a strain of the low back can be done by using active ROM and passive ROM (specifically active and passive SLR tests) as well as MR. The acronym commonly used to describe the care routine for an acute sprain or strain is RICE (rest, ice, compression, and elevation). RICE care should continue as long as inflammation is present in the tissues. This may be days, weeks, or even months or more—do not follow a cookbook rule for when to apply ice application. If inflammation is present, icing is appropriate.
Care for a chronic sprain is usually geared toward the tight muscles that usually occur as a compensation for the excessive motion. These tight muscles often cause pain and are in need of treatment. In addition, the best long-term approach that a client can take with a sprain is to strengthen the musculature of the region. Stronger musculature can compensate for the loss of stability of the stretched ligaments and help prevent painful muscle spasms.
Care for a chronic strain is geared toward loosening the muscles if they have become hypertonic and also eliminating or decreasing the formation of further adhesions. For this reason, once adhesions have mended the strained (torn) muscle tissue, and the tissue’s integrity has returned, it is important to begin soft tissue manipulation and stretching to minimize tightness and prevent the formation of further adhesions. If there is any doubt about whether tissue integrity has returned, consent from a physician should be obtained.
(Click here for a blog post article on sprains and strains of the low back and pelvis.)
Sacroiliac Joint Injury
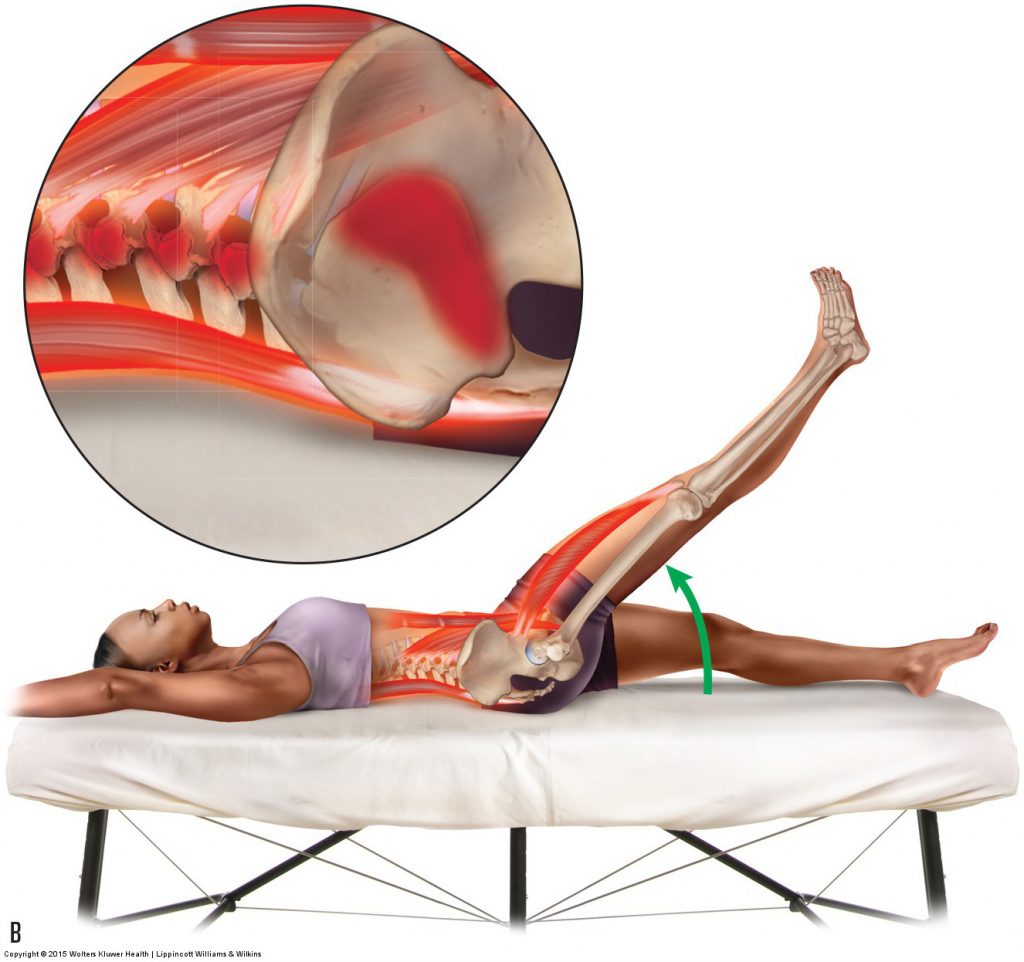
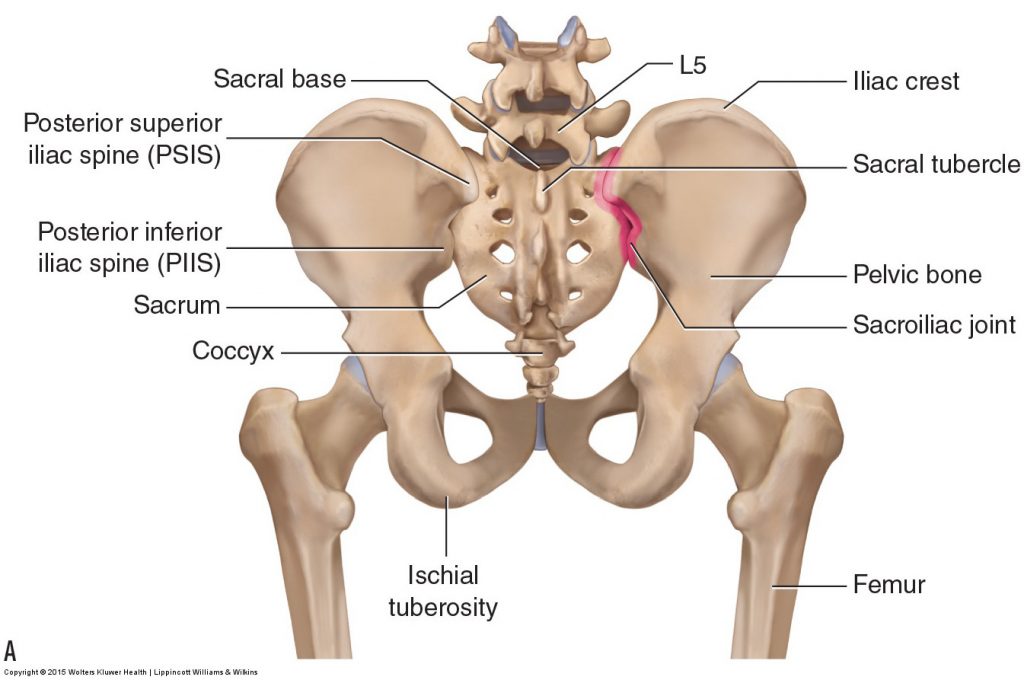 Injury (sprain, strain, or irritation/inflammation) to the sacroiliac joint (SIJ) can be assessed with active SLR test, passive SLR test, Nachlas’ test, Yeoman’s test, and the sacroiliac medley of tests. If either SLR test is used, injury to the SIJ will usually cause pain at approximately 30 degrees of thigh flexion. Nachlas’ test will usually only show positive if the injury is moderate or marked in degree; Yeoman’s test is more sensitive and will usually detect a mild SIJ injury. For the SIJ medley of tests to be considered positive, at least three of the five tests should elicit pain in the SIJ.
Injury (sprain, strain, or irritation/inflammation) to the sacroiliac joint (SIJ) can be assessed with active SLR test, passive SLR test, Nachlas’ test, Yeoman’s test, and the sacroiliac medley of tests. If either SLR test is used, injury to the SIJ will usually cause pain at approximately 30 degrees of thigh flexion. Nachlas’ test will usually only show positive if the injury is moderate or marked in degree; Yeoman’s test is more sensitive and will usually detect a mild SIJ injury. For the SIJ medley of tests to be considered positive, at least three of the five tests should elicit pain in the SIJ.
Care for a SIJ injury depends on what type of injury is present. SIJ sprains and strains should be treated similarly to lumbar sprains and strains (see preceding section). If no sprain or strain is present and the SIJ is simply irritated/swollen, then icing and rest are appropriate. Prolonged sitting, particularly prolonged driving, is especially stressful to the SIJs and should be eliminated or decreased.
(Click here for a blog post article on sacroiliac joint injury.)
Pathologic Disc and Sciatica
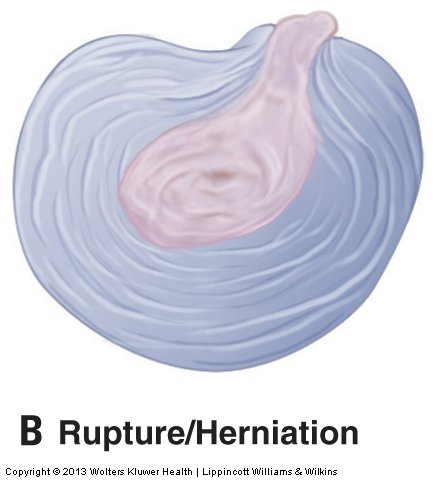 Assessing a pathologic lumbar (low back) disc condition (a disc bulge or rupture) and the resultant pressure on the sciatic nerve (sciatica) can only be done definitively by magnetic resonance imaging (MRI) or computed tomography (CT) scan. However, the SLR test, cough test, Valsalva maneuver, and slump test may also be used. Although these assessment procedures are not as accurate as an MRI, they are usually effective at accurately assessing a pathologic disc that is moderate or marked in severity. If a lumbar disc bulge or rupture is moderate or severe in presentation, it will likely produce a positive test result for most or all assessment procedures. However, a mild case may produce a negative result for many of the tests and a positive result for others. If there is any question about whether a client has a pathologic disc bulge or rupture, it is advisable to refer the client to a physician for a definitive diagnosis.
Assessing a pathologic lumbar (low back) disc condition (a disc bulge or rupture) and the resultant pressure on the sciatic nerve (sciatica) can only be done definitively by magnetic resonance imaging (MRI) or computed tomography (CT) scan. However, the SLR test, cough test, Valsalva maneuver, and slump test may also be used. Although these assessment procedures are not as accurate as an MRI, they are usually effective at accurately assessing a pathologic disc that is moderate or marked in severity. If a lumbar disc bulge or rupture is moderate or severe in presentation, it will likely produce a positive test result for most or all assessment procedures. However, a mild case may produce a negative result for many of the tests and a positive result for others. If there is any question about whether a client has a pathologic disc bulge or rupture, it is advisable to refer the client to a physician for a definitive diagnosis.
Treating a client with a lumbar disc problem contraindicates doing anything that would increase pressure on the disc, thereby increasing the size of the bulge or rupture. Strong compression over the spine should be avoided, and all movements of the client’s lumbar spine should be done with caution. As a rule, anything that increases the referral symptoms of the disc lesion is contraindicated. There are opposing viewpoints on what type of motions are safe and effective for a client with a lumbar disc injury. Some authorities recommend flexion motions and avoiding extension (or avoiding extension with lateral flexion if the disc injury is posterolateral); others recommend that the client perform extension motions and avoid flexion. The argument for flexion is that it opens up the vertebral and intervertebral foramina. The argument for extension is that it removes tension on the posterior annular fibers and pushes the nucleus pulposus anteriorly away from the posterior annular fibers.
The primary focus of manual therapy is to loosen the tight muscles that surround the disc because they can increase compression on the disc, furthering the problem. As a general rule, Western-based Swedish strokes are usually fine as long as the pressure is not so great that the vertebral joints are actually moved, thereby placing stress on the discs. Because of the movement involved in stretching and joint mobilization, these treatment techniques should be avoided or done prudently at or near the level of the disc lesion. Lumbar spine traction/distraction, if performed prudently, is indicated and can be beneficial for relieving disc pressure.
(Click here for a blog post article on pathologic disc conditions of the lumbar spine and sciatica.)
Piriformis Syndrome
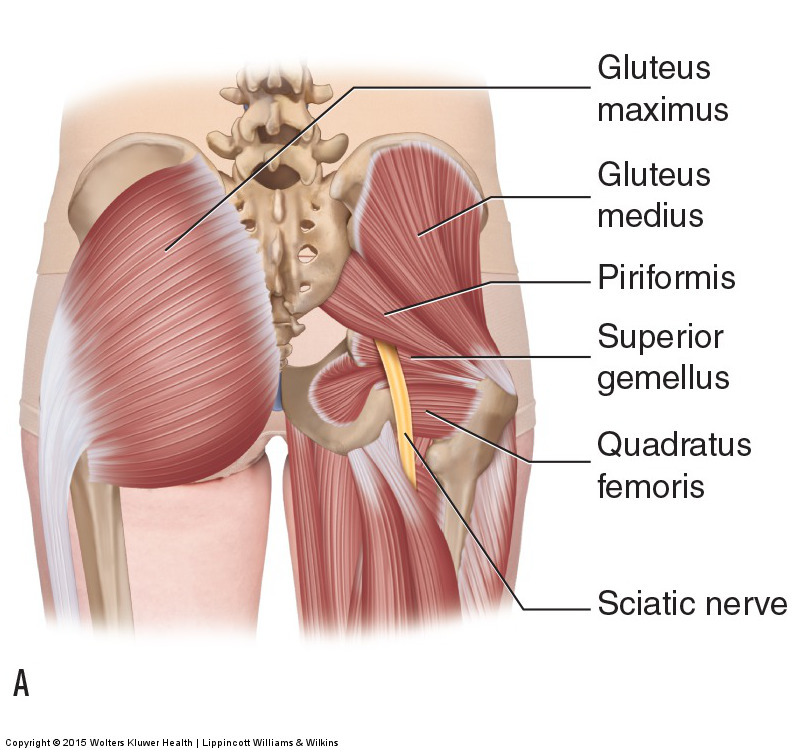 Piriformis syndrome is best assessed with the piriformis stretch test as well as palpation of the piriformis muscle. However, any of the assessment tests for pathologic discs or other space-occupying lesions may also show positive for piriformis syndrome. These tests include SLR, cough test, Valsalva maneuver, and slump test.
Piriformis syndrome is best assessed with the piriformis stretch test as well as palpation of the piriformis muscle. However, any of the assessment tests for pathologic discs or other space-occupying lesions may also show positive for piriformis syndrome. These tests include SLR, cough test, Valsalva maneuver, and slump test.
Treatment for piriformis syndrome is aimed at relaxing and loosening the piriformis muscle. Heat, soft tissue manipulation, and stretching are all effective means to accomplish this. If the piriformis is tight as a compensation to stabilize the sacrum when there is an underlying SIJ injury, resolving the SIJ condition is necessary if any lasting relief of the piriformis is to occur.
(Click here for a blog post article on piriformis syndrome.)
Degenerative Joint Disease
 Physicians assess low back degenerative joint disease (DJD; also known as osteoarthritis [OA]) by radiograph or other radiologic examination such as MRI or CT scan. Manually, DJD of the lumbar spine and SIJs is difficult to assess through palpation because the bone spurs of DJD are located deep within the client’s tissues. Advanced DJD will impede motion of the affected joints so passive ROM will be decreased and will often have a hard palpatory end-feel to the motions.
Physicians assess low back degenerative joint disease (DJD; also known as osteoarthritis [OA]) by radiograph or other radiologic examination such as MRI or CT scan. Manually, DJD of the lumbar spine and SIJs is difficult to assess through palpation because the bone spurs of DJD are located deep within the client’s tissues. Advanced DJD will impede motion of the affected joints so passive ROM will be decreased and will often have a hard palpatory end-feel to the motions.
There is nothing that a manual therapist can do to directly affect the bone spurs of DJD itself. However, manual therapy can play an extremely important role indirectly. The principal cause of DJD is physical stress to the joint, and one of the components of the physical stress is the compression force caused by tight muscles that cross the joint. If manual therapy relaxes tight musculature, less physical stress will be placed on the joint, and that can lead to a decrease or cessation in the rate at which the condition progresses. Therefore, even though manual therapy cannot reverse the condition, it can decrease its progression.
If the DJD is advanced and the client has a bone spur that is pushing on adjacent tissue, causing inflammation, another treatment option is the use of cryotherapy (the application of ice). If the bone spur is pressing on a spinal nerve, any positioning/stretching/joint mobilization that increases that nerve compression should be avoided.
(Click here for a blog post article on degenerative joint disease / osteoarthritis.)
Scoliosis
 If scoliosis is severe enough, it can be assessed through visual and palpatory examination. However, for a definitive diagnosis, radiographic examination via an x-ray should be ordered by a physician.
If scoliosis is severe enough, it can be assessed through visual and palpatory examination. However, for a definitive diagnosis, radiographic examination via an x-ray should be ordered by a physician.
Treatment of scoliosis by a manual therapist has two objectives: one is to work on the spinal joints and the other is to work the spinal musculature. Joint mobilization can be performed to increase motion of hypomobilities found within the scoliotic spine. Each vertebra within a scoliotic curve is laterally flexed and rotated. As a result, the vertebral segment will usually have decreased ROM in the opposite lateral flexion direction and also in the opposite rotation direction. The manual therapist can perform joint mobilization to decrease these hypomobilities. If the scoliosis is severe and/or very chronic, it is unlikely that joint mobilization will greatly reduce the degree of scoliosis, but it is often very effective at decreasing or stopping the progression of the condition.
Perhaps even more important is the role of the manual therapist in treating the associated spinal musculature. Asymmetric muscular pull can contribute to a scoliotic curvature by pulling the vertebrae in one direction. Therefore, the role of the manual therapist is to reduce muscular hypertonicities that can contribute to the problem. This can be done via heat, soft tissue manipulation, and stretching. If strengthening is within the therapist’s scope of practice, it should also be done. Although it is beneficial to relax and stretch as well as strengthen all musculature of a scoliotic curve, as a general rule, musculature in the concavity of the curve needs to be loosened, and musculature on the convex side of the curve needs to be strengthened.
(Click here for a blog post article on scoliosis.)
Anterior Pelvic Tilt and Hyperlordotic Lumbar Spine
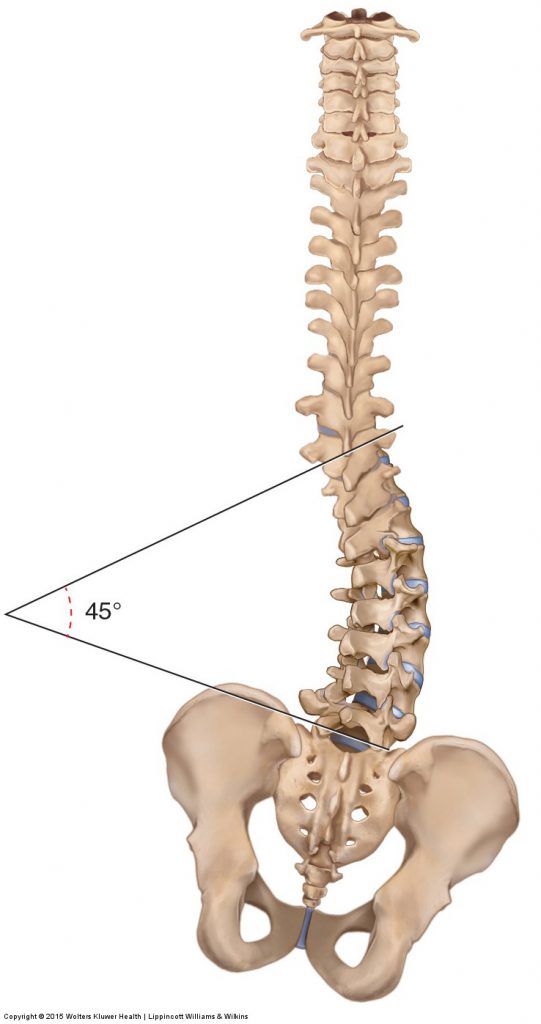
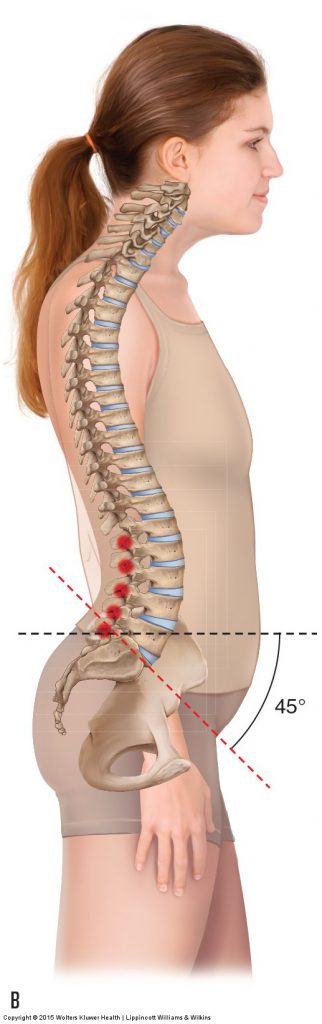
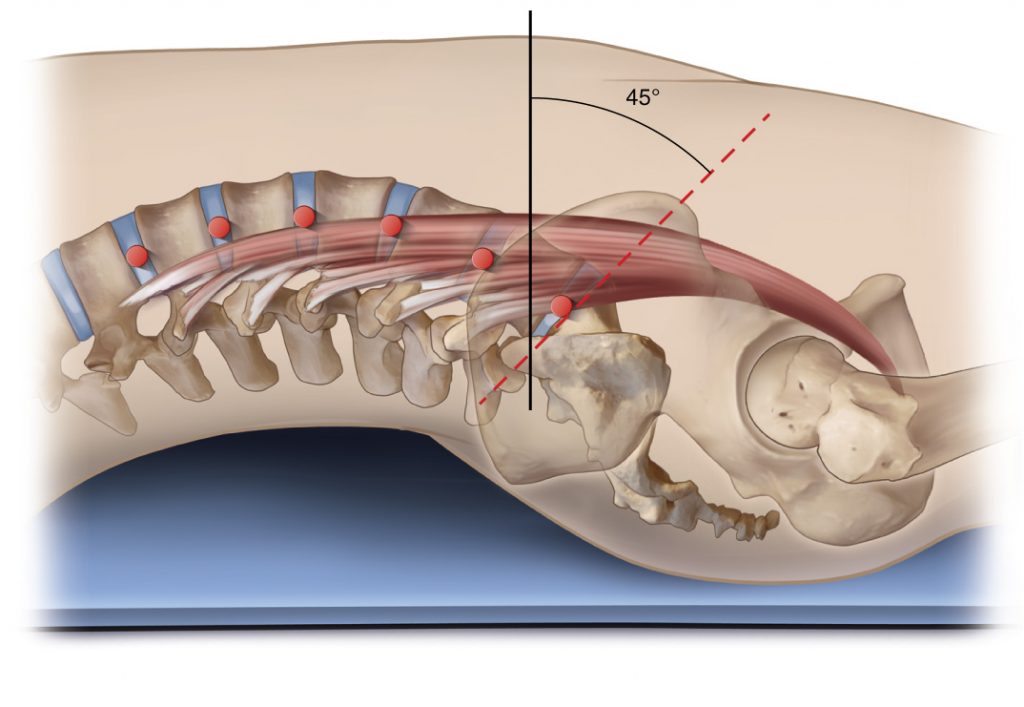 Anterior pelvic tilt and hyperlordotic lumbar curvature (lower crossed syndrome) can be assessed via visual examination. A more definitive diagnosis of the degree of the condition can be obtained via a physician-ordered radiograph (x-ray).
Anterior pelvic tilt and hyperlordotic lumbar curvature (lower crossed syndrome) can be assessed via visual examination. A more definitive diagnosis of the degree of the condition can be obtained via a physician-ordered radiograph (x-ray).
Treatment of this condition is aimed at loosening the anteriorly placed hip flexor musculature as well as the posteriorly placed low back extensor musculature. This can be accomplished by using heat, soft tissue manipulation, and stretching. If strengthening is within the therapist’s scope of practice, strengthening of the posterior hip extensor musculature and the anterior abdominal wall musculature should also be done. Although self-care is important in all conditions, it is especially important with dysfunctional postural patterns such as excessive anterior tilt. The client should be counseled regarding proper posture and stretches for the hip flexors and low back extensor muscles.
(Click here for a blog post article on lower crossed syndrome.)
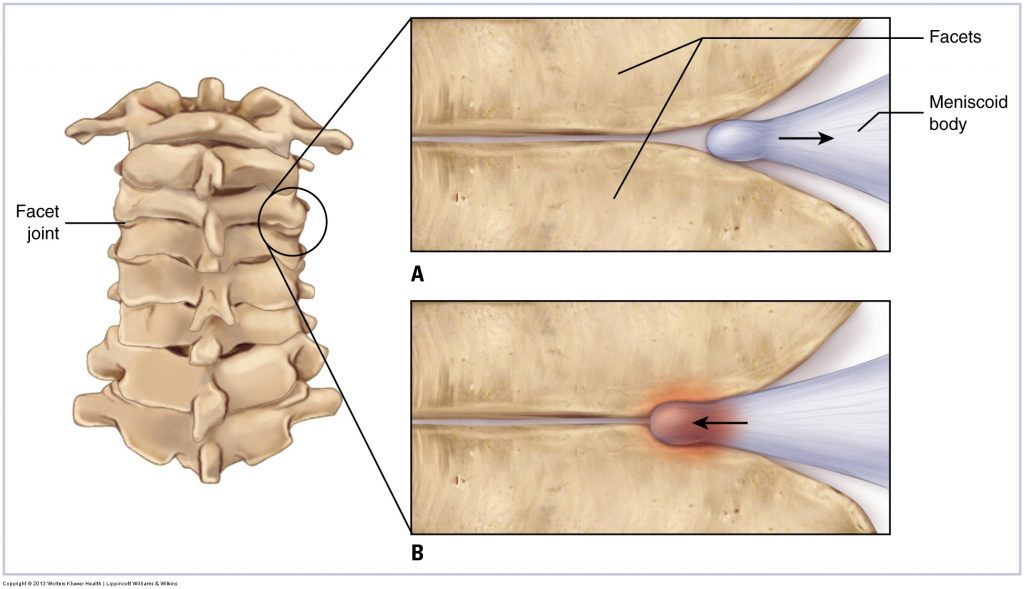
Facet Syndrome
 Facet syndrome is assessed by asking the client to perform extension of the lumbar spine; pain located at the spinal joints indicates facet syndrome.
Facet syndrome is assessed by asking the client to perform extension of the lumbar spine; pain located at the spinal joints indicates facet syndrome.
Because facet syndrome is often caused by excessive anterior pelvic tilt with resultant increased lumbar lordosis, treatment should be directed at improving the client’s posture. This can be best accomplished by applying moist heat, soft tissue manipulation, and stretching to the musculature of anterior tilt, in other words, the hip flexors and low back extensors. And if strengthening is within the therapist’s scope of practice, then strengthening of the posterior tilt musculature, hip extensors, and trunk flexors (anterior abdominal wall) should also be done. Self-care stretches that posteriorly tilt the client’s pelvis and flex the client’s lumbar spine should also be recommended. Because facet syndrome is often accompanied by muscular spasming, it is important to relax this musculature as well.
(Click here for a blog post article on facet syndrome.)
Spondylolisthesis
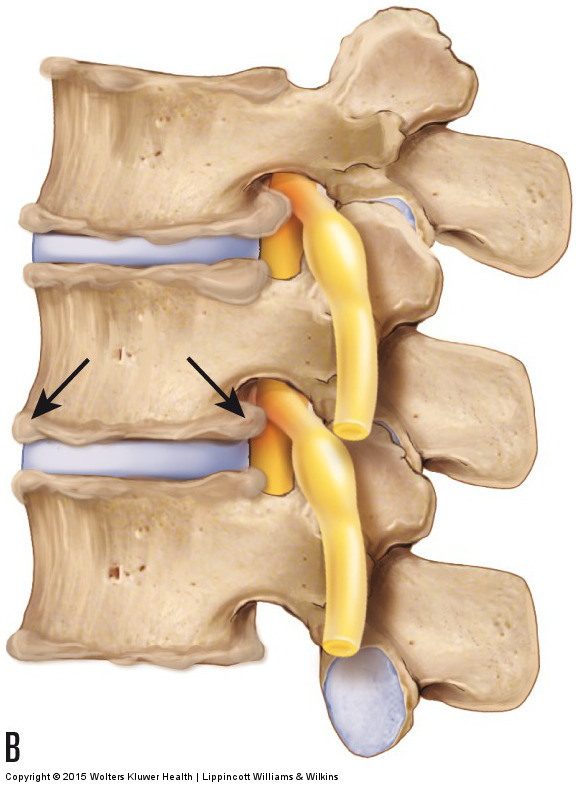
 Spondylolisthesis is diagnosed by a physician from lateral view radiographs. A break in the pars interarticularis and/or a slippage of one vertebra on the vertebra below indicates spondylolisthesis. By far, the most common type of spondylolisthesis involves an anterior slippage of the upper vertebra and is termed an anterolisthesis. Less common, the upper vertebra slips posteriorly and is termed a posterolisthesis, or slips laterally and is termed a laterolisthesis.
Spondylolisthesis is diagnosed by a physician from lateral view radiographs. A break in the pars interarticularis and/or a slippage of one vertebra on the vertebra below indicates spondylolisthesis. By far, the most common type of spondylolisthesis involves an anterior slippage of the upper vertebra and is termed an anterolisthesis. Less common, the upper vertebra slips posteriorly and is termed a posterolisthesis, or slips laterally and is termed a laterolisthesis.
Manual therapy treatment of a spondylolisthesis cannot change the break in the pars interarticularis. Instead, treatment is aimed at reducing any associated muscle spasm and increasing the stability of the lumbar spine through core stabilization strengthening, if this is within the therapist’s scope of practice. Muscle spasm is best reduced via moist heat, soft tissue manipulation, and stretching. Core stabilization strengthening should be directed toward the anterior abdominal wall musculature as well as the low back extensor muscles.
Because an excessive lumbar lordotic curve, often caused by excessive anterior tilt of the pelvis, exacerbates the slippage of an anterolisthesis, remedying this postural condition through hands-on care and self-care advice (see the previous section on “Anterior Pelvic Tilt and Hyperlordotic Lumbar Spine”) is an important component of the care of this condition.
(Click here for a blog post article on spondylolisthesis.)
This blog post article is the 18th in a series of 18 blog posts on the subject of assessment of the low back and pelvis.
The blog post articles in this series are:
- Introduction to Assessment of the Low Back and Pelvis
- Health History
- Introduction to Physical Assessment Examination of the Low Back and Pelvis
- Postural Assessment of the Low Back and Pelvis
- Range of Motion and Manual Resistance Assessment of the Low Back and Pelvis
- Muscle and Bone Palpation of the Low Back and Pelvis
- Joint Motion Palpation Assessment
- Overview of Special Orthopedic Assessment Tests of the Low Back and Pelvis
- Straight Leg Raise Tests for Space-Occupying Lesions
- Cough Test and Valsalva Maneuver
- Slump Test
- Piriformis Stretch Test
- Straight Leg Raise and Manual Resistance Tests for Strains and Sprains
- Nachlas and Yeoman’s Tests
- Sacroiliac Joint Medley of Tests
- Treatment Strategy for the Low Back and Pelvis
- Self-Care Advice for the Client with a Low Back / Sacro-Iliac Joint Condition
- Brief Review of Assessment and Treatment of Conditions of the Low Back and Pelvis


