What are Fascial Adhesions?
 Fascial adhesions, also known as scar tissue adhesions (or fibrous adhesions, or more simply adhesions), are composed of fibrous fascia collagen fibers (see accompanying figure). These collagen fibers are the same substance that makes up tendons, ligaments, and other fibrous fascial tissues. Although adhesions are normally thought to be deposited in sites of trauma (i.e., scar tissue), they are in fact deposited continuously between the soft tissues of the body. These fibers increase the stability of the tissues by binding/connecting the tissues together. However, if adhesions buildup excessively, they may bind together the two opposing surfaces of a soft tissue interface, which should slide along one another when movement is needed, resulting in restricted mobility. In a client with an active lifestyle, these fibers do not get the chance to buildup because as the client’s body moves, adhesions that have formed are broken up and resorbed. However, a sedentary lifestyle encourages adhesions to buildup progressively until mobility is greatly restricted. Although adhesions do not actually cause an increase in the baseline resting tone contraction level of a muscle, they do add to the muscle’s tightness by decreasing the muscles’ ability to stretch and lengthen. If a muscle cannot lengthen, then it cannot allow movements of the body performed by the antagonists to that muscle.
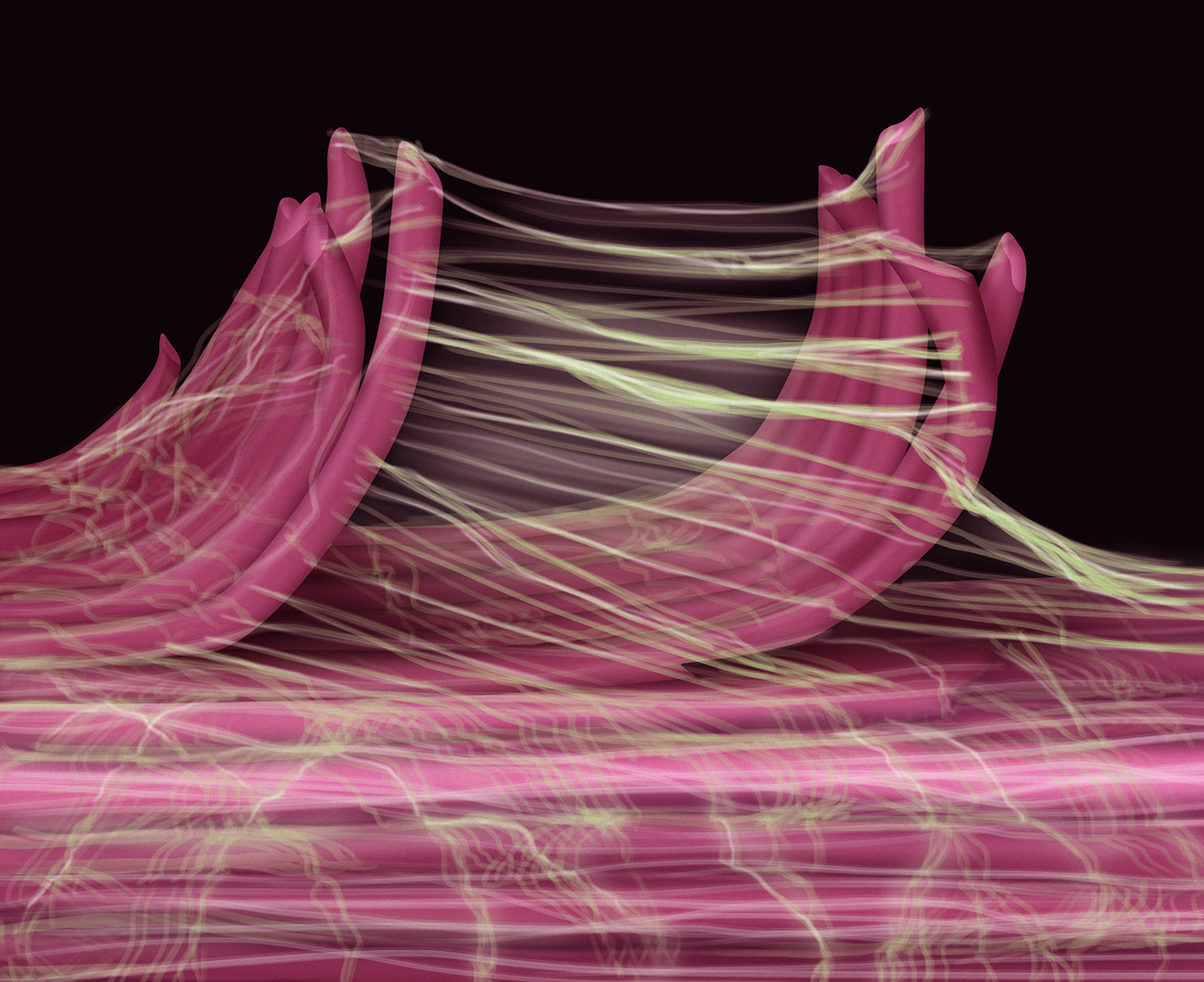
Fascial adhesions, also known as scar tissue adhesions (or fibrous adhesions, or more simply adhesions), are composed of fibrous fascia collagen fibers (see accompanying figure). These collagen fibers are the same substance that makes up tendons, ligaments, and other fibrous fascial tissues. Although adhesions are normally thought to be deposited in sites of trauma (i.e., scar tissue), they are in fact deposited continuously between the soft tissues of the body. These fibers increase the stability of the tissues by binding/connecting the tissues together. However, if adhesions buildup excessively, they may bind together the two opposing surfaces of a soft tissue interface, which should slide along one another when movement is needed, resulting in restricted mobility. In a client with an active lifestyle, these fibers do not get the chance to buildup because as the client’s body moves, adhesions that have formed are broken up and resorbed. However, a sedentary lifestyle encourages adhesions to buildup progressively until mobility is greatly restricted. Although adhesions do not actually cause an increase in the baseline resting tone contraction level of a muscle, they do add to the muscle’s tightness by decreasing the muscles’ ability to stretch and lengthen. If a muscle cannot lengthen, then it cannot allow movements of the body performed by the antagonists to that muscle.
Note: Treatment Considerations in Brief for Fascial Adhesions of the Neck:
The mobility of cervical spinal ligaments, joint capsules, and all other soft tissues of the neck can be affected by adhesions as well. Manual therapy treatment techniques for the neck such as massage, stretching, and hydrotherapy all help to break up adhesions in muscles and other soft tissues. Joint mobilization serves to break up patterns of adhesions in the intrinsic fascial tissues (ligament/joint capsule complex) of the cervical spinal joints.
As a general rule, with any manual therapy treatment to the neck, there are always precautions and contraindications to consider given the number of sensitive structures present.
Fascial collagen fibers have a spiderweb appearance. Educator and author, Gil Hedley, uses the term fuzz to describe fibrous fascia. Figure courtesy of Joseph E. Muscolino, Drawn by Giovanni Rimasti, based on a Photo by © Ronald A. Thompson.
Note: This blog post article is the first in a series of 10 posts on
Common Musculoskeletal* Conditions of the Neck
The 10 Blog Posts in this Series are:
- Fascial Adhesions (and an introduction to musculoskeletal conditions of the neck)
- Hypertonic (tight) musculature
- Joint dysfunction
- Sprains and strains
- Pathologic disc conditions
- Osteoarthritis (OA)
- Thoracic outlet syndrome (TOS)
- Forward head posture
- Tension headaches
- Greater occipital neuralgia
(*perhaps a better term is “neuro-myo-fascio-skeletal”)
Introduction to Common Musculoskeletal Conditions of the Neck
Proper therapeutic treatment of a client’s neck depends on an accurate assessment of the client’s/patient’s condition(s) as well as a clear understanding of the mechanism of the pathologic condition(s) that the client is experiencing. Therefore, this series of 10 blog articles offers a brief description of the most common pathologic musculoskeletal conditions that affect the neck. My next blog post series will discuss the manual therapy assessment techniques used to assess these conditions.
When treating a healthy or unhealthy neck, it is most important to understand the mechanism, or physiology, of how the neck functions. Normal mechanics of the neck were addressed in our last series of blog posts. However, when a person has a pathologic condition, the mechanics of the neck are altered. Each pathologic condition has a unique physiologic mechanism, pathophysiology or pathomechanism, that, when understood, can guide critical reasoning regarding the therapeutic tools that should be used. Rather than asking the learner to apply a memorized “cookbook” routine from one technique or another that may be ineffective or perhaps even hurt the client, these blog posts will encourage learning how to choose the technique protocols that will safely and most effectively help the client.


