Sprains and strains of the low back and pelvis are usually addressed together because they are similar in nature. Technically, when a ligament or joint capsule is torn, it is termed a sprain; when a muscle is torn, it is termed a strain (Fig. 7).
Note: This blog post article is the fourth in a series of twelve articles on musculoskeletal conditions of the low back (lumbar spine) and pelvis. For the rest of the articles in the series, scroll to the end of this article.
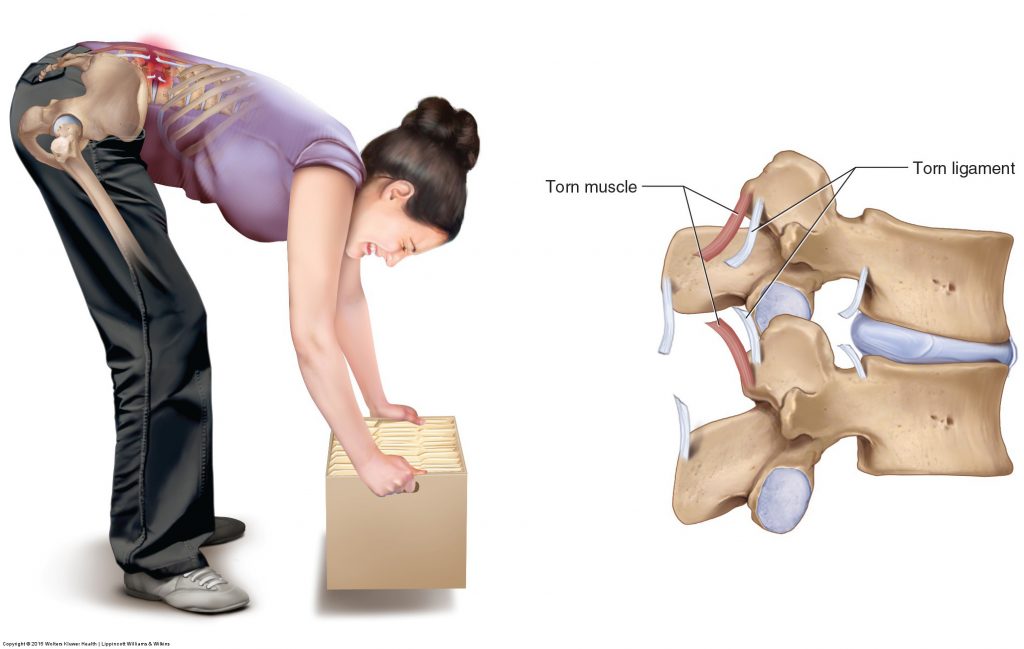
Figure 7. Low back strain and sprain. Attempting to lift a heavy object that is in front of the body places a strong force on the posterior tissues of the low back. If this force is excessive, a tearing of the low back extensor musculature, termed a strain, can occur. A tearing of ligament, termed a sprain, can also occur. Permission Joseph E. Muscolino. Manual Therapy for the Low Back and Pelvis – A Clinical Orthopedic Approach. 2015.
Description of Sprains and Strains of the Low Back and Pelvis
Sprains and strains tend to occur together because the force that is necessary to tear one tissue will likely cause tearing of the other. However, sprains and strains are not always equally present. An injury may present as a minor sprain but be a major strain or vice versa. The severity of a sprain or a strain is expressed as follows:
- Grade I: minor tear
- Grade II: moderate tear
- Grade III: marked tear or complete rupture
Note: The term strain is often used loosely. At times, a client who is described as having a strain actually has a muscle spasm. As explained previously, when a muscle is stretched too quickly or too far, the muscle spindle’s stretch reflex is initiated, which causes the muscle to contract (spasm). This reflex prevents the muscle from being torn and therefore strained. However, the resulting muscle spasm is often described as a strain (certainly, if some tearing occurred before the stretch reflex engaged, then it would truly be a strain in addition to a spasm). However, it is possible to justify the use of the term strain in this scenario from another perspective. Any strenuous use of a muscle usually results in a normal and healthy amount of microtearing of the muscle’s fascial tissue. This fascial microtearing is necessary so that the fascia can mend and heal larger. This allows for more sarcomeres and sarcoplasm to be placed in the muscle fiber when a muscle hypertrophies after exercising. Hence, this microtearing could be interpreted as a minor strain of the muscle. The most important point is to understand the mechanism of what is occurring so that treatment is appropriate for the condition.
Given that strains and sprains involve torn soft tissue, pain, inflammation, and bruising are usually present when the sprain and/or strain are in the acute stage. Muscular splinting/spasming is also present in the acute stage and often persists long-term.
Although sprains and strains are similar, functionally, they present quite differently. Sprains are worse than strains because ligaments lack a good blood supply and therefore do not heal well. For this reason, once a ligament has been stretched and torn, it usually heals stretched out and remains that way for the rest of the client’s life, resulting in chronic joint hypermobility. Musculature, on the other hand, has a good blood supply, so strains usually heal well if properly treated. However, the presence of a good blood supply also causes more bleeding and bruising with strains. Strains also usually hurt more than sprains because muscle tissue has more sensory nerve endings than ligaments.
Mechanism and Causes of Sprains and Strains of the Low Back and Pelvis
The mechanism for sprains and strains is similar. An excessive pulling force causes a disruption of the fibers of the ligament or musculature (see Fig. 7). This pulling force can occur during a macrotrauma, such as bending over to lift a heavy object, a fall, or a car accident. It can also occur from repeated postural or movement microtraumas, such as overuse injuries that place excessive tension on ligaments and muscles over time; repeated bending is a good example of this. Given that ligaments only become taut at the end range of motion, low back sprains tend to occur at the end range of a motion. Low back strains, on the other hand, while they can occur at the end range of motion, they can also occur anywhere during the range of motion. So asking the client at what point during their motion that the pain occurred can often help discern between a sprain and strain. Of course, they often occur together to some degree.
The function of a ligament is to limit motion of a joint; therefore, if the ligament is torn and stretched, the joint tends to become hypermobile and less stable. This may be masked during the acute phase by muscular splinting/spasming. Strains, on the other hand, tend to result in joint hypomobility, both because of muscular spasming that occurs in the short run and often continues into the long run, as well as the formation of scar tissue adhesions that occur during the healing process. Although adhesions are necessary to repair and mend torn soft tissues, if excessive adhesions are allowed to form, the tissue will lose its mobility, resulting in decreased ranges of motion.
Note: Treatment Considerations in Brief for Sprains and Strains of the Low Back and Pelvis
Icing is especially useful for treating acute strains and sprains. Massage is helpful for sprains and strains when the condition is subacute and/or chronic. Stretching is helpful for subacute and chronic care of strains.
This blog post article is the fourth in a series of twelve articles on musculoskeletal conditions of the low back (lumbar spine) and pelvis.
The articles in this series are:
- Hypertonic / tight muscles
- Myofascial trigger points
- Joint dysfunction
- Sprains and strains
- Sacroiliac joint injury
- Pathologic disc conditions and sciatica
- Piriformis syndrome
- Degenerative joint disease (DJD)
- Scoliosis
- Lower crossed syndrome
- Facet syndrome
- Spondylolisthesis


