This blog post article is part of a series of articles on assessment of the low back and pelvis. Scroll to the end of this article to see the others in this series.
Health History
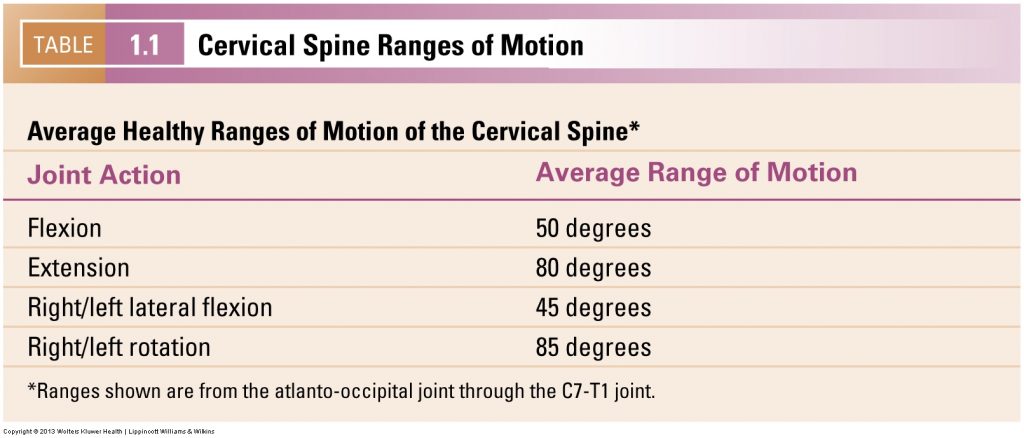
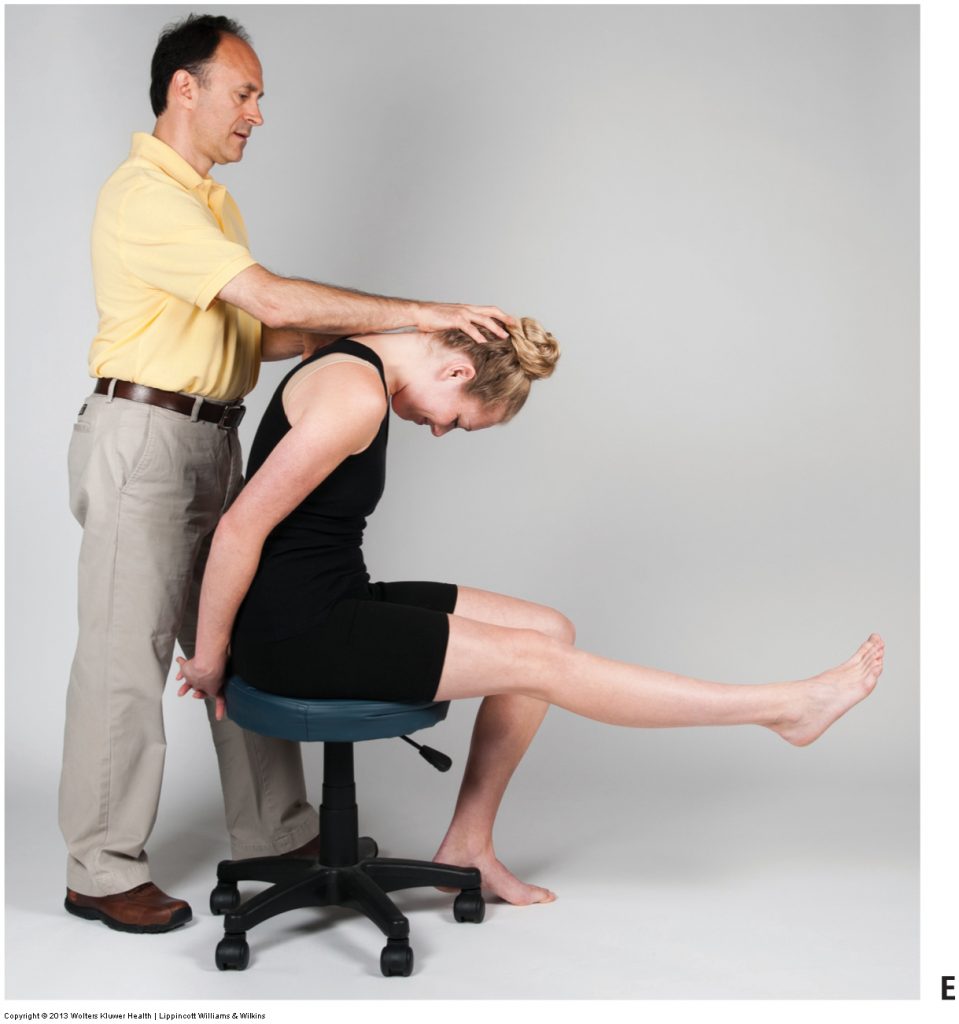
Cervical spine ranges of motion. Permission Joseph E. Muscolino. Advanced Treatment Techniques for the Manual Therapist: Neck (2013)
Think of the health history as a conversation between the therapist and the client. The health history may begin by having the client complete a written questionnaire about the present condition as well as his or her past health history. The conversation continues with a verbal history in which the client answers additional questions regarding his or her health.
The health history is usually done before the physical assessment exam because it helps reveal the problem regions that need to be assessed during the physical exam. If the history is thorough enough, the signs and symptoms discussed during the conversation will often indicate the client’s condition or conditions, allowing the examination to be more focused and efficient. During the history, there is no one required order to the questions asked, however, it may be helpful to the individual therapist to develop and follow a consistent order when conducting health histories. Such consistency not only helps keep thoughts organized but also increases efficiency when returning later to review a client’s information. However, it is also important to be flexible with questions. The client’s answer to one question will often determine the follow-up questions. Although it is impossible to state every question that should be asked during a health history, some of the key questions are listed below.
Health History Questions
- What are your height and weight?
- Are you right-hand or left-hand dominant?
- What is the problem area?
- When did symptoms first begin?
- What precipitated the problem? Was there a trauma or did it begin insidiously?
- Have you had this problem before?
- Have you had any other problems with your low back or pelvis before?
- If there is pain, is the quality of the pain sharp or dull?
- On a scale of 0 to 10, where 0 is no pain at all and 10 is the worst pain you can imagine having, what number would you assign your pain level?
- Are there shooting pains or other referral of symptoms down into the lower extremities (buttock, thigh, leg, or foot)?
- Are the symptoms (pain or other symptoms) related to the time of day? If so, is it worse first thing in the morning or at the end of the day?
- Are the symptoms related to certain postures or activities?
- Does the pain increase with prolonged standing or prolonged sitting?
- Are there other precipitating factors that cause the symptoms?
- What increases the symptoms? What decreases the symptoms?
- Overall, since the problem began, is the severity getting better, worse, or staying the same?
- Have you had this condition treated yet? If so, by whom? What was their assessment/diagnosis? What was their treatment? What was your progress with this treatment? May I have written permission to contact the therapist/physician about your treatment?
- What do you think is the cause of your condition?
In addition to questions that are specific to the client’s presenting complaint, it is also valuable to gather information about the client’s general health.
- Do you have any other health conditions, musculoskeletal, or otherwise?
- What is your history of broken bones/fractures, car accidents, and other physical traumas?
- Are you on any medications? Do you take them regularly, or are they only for a temporary condition?
- How much do you exercise?
- What postures (at work and home) do you assume most often?
- In what position(s) do you sleep?
- Do you smoke? Do you drink alcohol? If so, how much, and how often?
- What is your stress level?
- Is there a family history of musculoskeletal problems?
- Is there anything else that you would like to add that I have not asked about?
Differential Diagnosis / Differential Assessment
There was a popular TV show named House that ran for many years. House was a curmudgeon but brilliant physician who excelled at differential diagnosis. His method, when confronted with a new patient with a strange disease, was to assemble his team of physicians and write on a poster board the sign or symptom of the new patient. He and his team would then list every possible condition that could cause that sign/symptom. Their role toward differential diagnosis was to then, with verbal history, physical exam (or treatment) to rule in or rule out each of the conditions that they had listed. In a perfect world, everything but one condition would be ruled out, and the remaining condition would have to be the condition that the patient had. This is the essence of differential diagnosis. Of course, in a real world scenario, our patient/client usually presents with multiple signs and symptoms, so the list of possible conditions expands exponentially, and in the end, it is often found that they have multiple conditions. But again, this is the essence of differential diagnosis / differential assessment. The second we begin the verbal history with the person, we should start to create a list in our mind of every possible condition that could cause each sign or symptom that the person has. Our continuing history and our examination process (as well as treatment to see their response) should then be aimed at ruling in or ruling out each of the conditions on that list.
This blog post article is the 2nd in a series of 18 blog posts on the subject of assessment of the low back and pelvis.
The blog post articles in this series are:
- Introduction to Assessment of the Low Back and Pelvis
- Health History
- Introduction to Physical Assessment Examination of the Low Back and Pelvis
- Postural Assessment of the Low Back and Pelvis
- Range of Motion and Manual Resistance Assessment of the Low Back and Pelvis
- Muscle and Bone Palpation of the Low Back and Pelvis
- Joint Motion Palpation Assessment
- Overview of Special Orthopedic Assessment Tests of the Low Back and Pelvis
- Straight Leg Raise Tests for Space-Occupying Lesions
- Cough Test and Valsalva Maneuver
- Slump Test
- Piriformis Stretch Test
- Straight Leg Raise and Manual Resistance Tests for Strains and Sprains
- Nachlas and Yeoman’s Tests
- Sacroiliac Joint Medley of Tests
- Treatment Strategy for the Low Back and Pelvis
- Self-Care Advice for the Client with a Low Back / Sacro-Iliac Joint Condition
- Brief Review of Assessment and Treatment of Conditions of the Low Back and Pelvis


