Self-Care for the Client/Patient with Upper Crossed Syndrome

Extension on a physioball. Permission Joseph E. Muscolino.
When working with a client/patient for the treatment of upper crossed syndrome (named by Vladimir Janda), the importance of client/patient self-care is critical. First, the client/patient must be advised to avoid collapsing into the upper crossed rounded posture as much as possible. However, given the initial weakness of the shoulder girdle retractors and thoracic extensors with which they will present, it is important to explain to them that improving their posture will take time and patience. Therefore, they should not expect to suddenly sit and stand totally upright. Rather, it will be a gradual transition from their present posture to “ideal” posture as the facilitated/tight muscle groups are gradually loosened and the inhibited/weak muscle groups are gradually strengthened.
A good postural habit to recommend from the beginning is to stand whenever possible with the hands on the hips or clasped behind the back. This will passively increase shoulder girdle retraction and thoracic extension, without exhausting the still weak muscles of shoulder girdle retraction and thoracic extension. Standing with the hands on the hips also passively increase lateral (external) rotation of the arms at the glenohumeral joints. (Note: When standing with the arms behind the back, to minimize medial rotation of the arms, instruct the client/patient how to pronate the forearms at the radioulnar joints instead of medially/internally rotating the arms at the glenohumeral joints.)
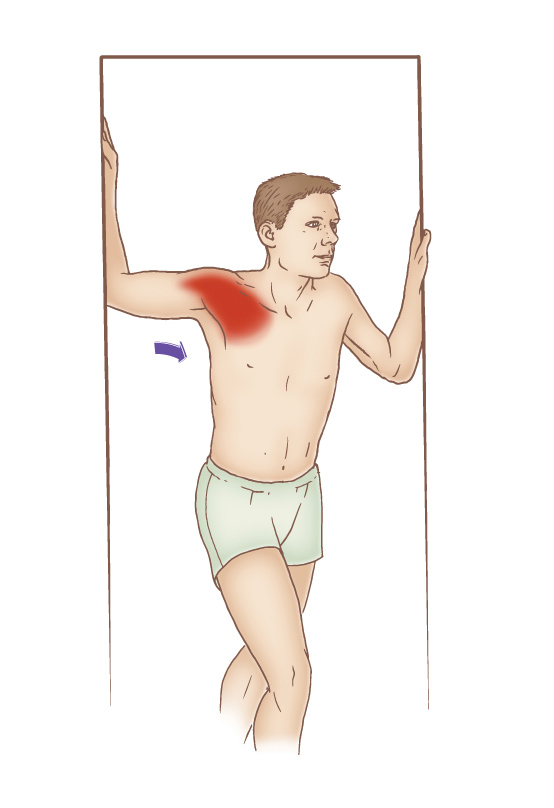
Self-care pectoralis stretch performed in a doorway. Permission: Joseph E. Muscolino, The Muscle and Bone Palpation Manual – with Trigger Points, Referral Patterns, and Stretching, 2ed (Elsevier, 2016).
Next, be sure to discuss with the client/patient all the scenarios in which they might be collapsing into the upper crossed posture. These might include sitting posture at a computer, driving a car, or most any activity in which the client/patient works down and in front of the body.
It is also important to recommend moist heat followed by stretching of the pectoralis musculature and upper thoracic spine. When stretching the pectoralis musculature in a doorway, it is helpful to place the hand/forearm against the doorframe at various heights so that different aspects of the pectoralis musculature are preferentially stretched. Having the upper arm horizontal best stretches the sternocostal head of the pectoralis major; placing the hand/forearm lower preferentially stretches the clavicular head of the pectoralis major; and placing the hand/forearm higher preferentially stretches the pectoralis minor. Also, note that the foot that steps forward should be same-side foot as the side being stretched. Asking the client/patient to rotate the trunk away from the doorframe further increases the stretch to the pectoralis musculature.
Stretching the thoracic spine across an exercise ball should be done with the feet stabilized against a wall for balance. Using a larger ball (perhaps 65 cm) at first creates a gentle stretch. Then transitioning to a smaller ball (perhaps 55 cm) increases the stretch into extension. Recommend to the client/patient to begin this stretch with repetitions of 5-10 seconds and gradually increase to holding the stretch for 30 seconds or more.
Finally, self-care exercises for strengthening are just as important as the moist heat and stretching component. Strengthening should be directed at the inhibited weaker musculature listed in Table 1 of an earlier blog post on this condition. Following are the five primary objectives of the strengthening program: 1. Retraction exercises aimed at the rhomboids and middle and lower fibers of the trapezius; 2. Strengthening the serratus anterior as a protractor in place of the pectoralis musculature; 3. Strengthening the deep cervical flexors in place of the SCM and scalenes (this is often obtained by making sure that the chin is somewhat tucked when performing neck flexion); 4. Strengthening the lateral rotation musculature of the GH joint; and 5. Strengthening the thoracic extensor musculature.
Medical Approach to Upper Crossed Syndrome
Upper crossed syndrome is a postural dysfunction pattern. As such, there really is no “medical” approach. Typically, if a medical doctor addresses this condition, it would be to refer the patient to physical therapy. Physical therapy would likely work with the patient with the same objectives of stretching and strengthening the musculature advocated here; moist heat and manual therapy might also be done. In addition, physical therapy modalities such as ultrasound and electrical muscle stimulation might also be performed for the facilitated/tight musculature.


