Tendon Pain
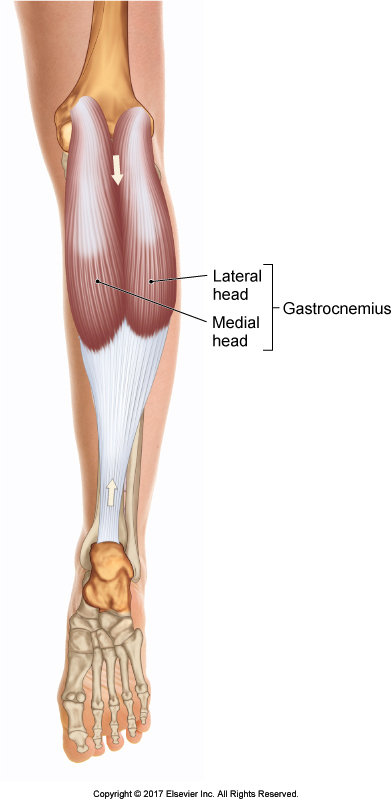
Permission Joseph E. Muscolino. The Muscular System Manual – The Skeletal Muscles of the Human Body, 4th ed. (Elsevier, 2017).
Tendon pain and dysfunction are the presenting clinical features of tendinopathy. Research has shown that treatment should be active (e.g., exercise-based), and an ongoing rehabilitation program is required. Dr. Jill Cook from La Trobe University shared in an editorial published in the British Journal of Sports Medicine: 10 things to avoid if you have lower limb tendon pain.
-
Don’t Rest Completely
Use it or lose it applies to tendons. Rest decreases the load tolerance of tendon, and complete rest decreases tendon stiffness within two weeks. It also decreases strength and power in the muscle attached to the tendon and likely changes the brain’s motor cortex, leaving the person less able to tolerate load at multiple levels. Treatment should initially reduce painful, high tendon load (e.g., jumping) and introduce beneficial loads (e.g., isometrics). Once the tendon pain is low and stable (consistent on a loading test each day), load can be increased slowly to improve the capacity of the tendon.
-
Don’t Prescribe Incorrect Exercise
Treatments that do not address the need to increase the ability of the tendon to take load are usually not helpful in the long term toward decreasing tendon pain, although they might give short-term pain relief. Correct exercise prescription needs to be based on an understanding of loading the tendon. Tendon must be loaded to be effective, so slow exercises with weights can be used early in rehabilitation. However, exercising at a longer muscle-tendon length (i.e., the muscle-tendon unit being stretched long) can compress the tendon at its bony insertion. This adds substantial load and should be avoided, even slowly, early in rehabilitation.
-
Don’t Use Passive Treatments
Passive treatments are not helpful in the long term toward reducing tendon pain as they promote the patient as a passive recipient of care and do not increase the load tolerance of tendon. Treatments like electrotherapy and ice will only temporarily ameliorate pain only for it to return when the tendon is loaded.
– Note by Joseph Muscolino. I believe this statement is far too strong. Advocating the use of active loading exercises does not preclude the use of passive manual and physical therapies. They are not mutually exclusive. Active and passive approaches can be mixed together into a treatment approach. (See another note of mine farther down this article for more on this.)
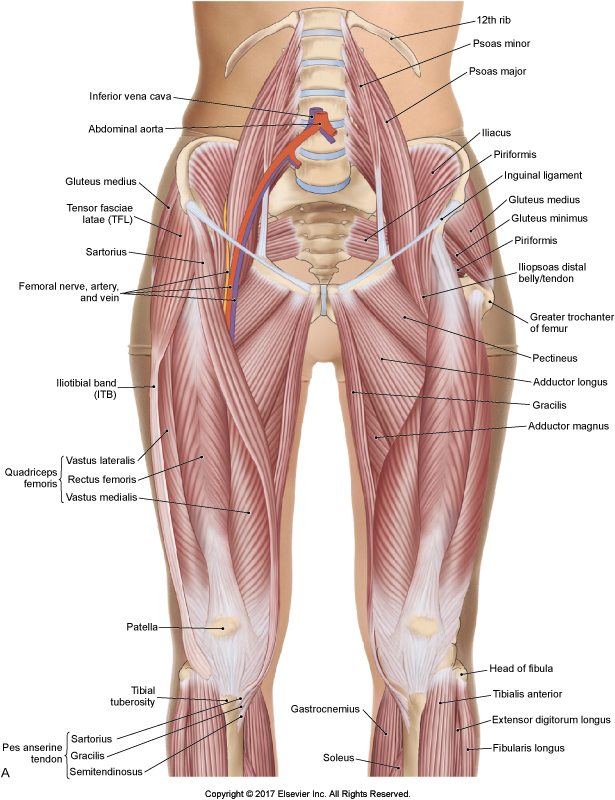
Hip Flexor Region. Permission Joseph E. Muscolino. The Muscular System Manual, The Skeletal Muscles of the Human Body, 4th ed. (Elsevier, 2017).
-
Avoid Injection Therapies
Injections of substances into a tendon have not been shown to be effective in good clinical trials. “Injections may change pain in the short term as they may affect the nerves, but should only be considered if the tendon has not responded to a good exercise-based program”
– Note by Joseph Muscolino: I have a problem with this statement for a couple of reasons. First, what type of injection therapies are we talking about? Cortisone, which clearly has negative side effects and should be avoided whenever possible? Or natural “regenerative” injections such as PRP (platelet rich plasma), which is simply our own plasma and platelets, which are spun down from our blood and then injected back into our body, and work by stimulating growth of new collagen in the degenerated tendon? Second, I believe that we are far too early in the process of gathering evidence to make such a strong statement. The absence of evidence-based proof does not prove the absence of efficacy. I love research, but it should not be an excuse to shut off our critical reasoning skills. Instead, it makes sense to use critical reasoning and our understanding of anatomy and physiology to determine if a particular treatment might be of benefit. Yes, we cannot be sure yet, but using the body’s own platelets to kick start a healing process of fascial connective tissue makes sense, both for its likely benefits and unlikely chance of negative side effects. And from the early studies I have seen, it seems that regenerative therapy does seem to be effective. Further, using regenerative injections does not preclude using active treatment approaches such as the ones recommended here.
-
Don’t Ignore Your Pain
Pain is a way of telling you that the load is too much. Tendon pain usually increases 24 hours after excess tendon load. An increase in pain of two or more points (out of 10) on a daily loading test is a sign of overloading the tendon, which may be due to excessive spring-like movements such as jumping or running and changing direction.
-
Don’t Stretch Your Tendon
Aside from the load on your tendon when you play sport, there are compressive loads on the tendon at the bone-tendon junction when the tendon is at its longest length. Stretching only serves to add compressive loads that are detrimental to the tendon. Stretching while you are standing can be especially provocative to the tendon.
– Note by Joseph Muscolino: I do not necessarily disagree with this statement except to say that there might be other factors to consider. For example, stretching might be indicated to stretch concomitant muscle tightness and/or maintain joint flexibility. It is rare for a patient/client to present with one isolated problem, in other words, with only one tissue dysfunction such as tendon injury. When presented with multiple tissue dysfunctions, we often we need to make clinical judgments regarding the relative efficacy of a treatment option based on its positive effects on one tissue versus its negative effects on another tissue.
-
Don’t Massage Your Tendon
A tendon that is painful is one that is telling you that it is overloaded and irritated, therefore massaging or frictioning it can actually increase your pain. Sometimes tendons will feel better immediately after a massage but can then be worse when you load them. Massage of the attached muscle can be helpful.
– Note by Joseph Muscolino: I am not a big advocate of forceful transverse friction techniques, perhaps because I believe that regenerative injection therapies can accomplish more improvement, more quickly, and with far less associated pain (see my note above). But the efficacy of stimulating degenerated fascial tissue (e.g., tendinosus) seems pretty clear. It is usually stated that deep tissue work, for example transverse friction, should not be used as a treatment for an acute tendinitis, but should be used for a chronic tendinosus. The problem is that it is not as if a switch is flipped and an acute tendinitis suddenly becomes a chronic tendinosus. There is often a long transition period in which a tendon is both inflamed (itis) and degenerated (osus), in other words, there is tendinitis and tendinosus occurring at the same time. And pain is often present for much or all this time. Certainly, I agree that pain is a signal that the body either has tissue damage, or the nervous system believes that damage is likely to occur (of that there could simply be pain sensitization). And the wisdom of the body should be listened to. But following this rule too rigidly would seem to indicate that all manual and movement therapies would be totally free of pain or discomfort. I am only trying to qualify this statement. In the end, a therapist should choose the appropriate treatment tools based on the likelihood that they will help to heal the pathomechanics of the condition with which the patient/client presents.
Anterior view of the knee joint bilaterally. Permission Joseph E.Muscolino. www.learnmuscles.com.
-
Don’t Use Tendon Images for Diagnosis, Prognosis, or as an Outcome Measure
The pictures of your tendon with ultrasound and MRI can frighten you, and the words used by doctors such as degeneration and tears can make you wonder if your tendon should be loaded. There is good evidence that the pathological tendon can tolerate loads, especially when you gradually increase the loads on them.
– Note by Joseph Muscolino: Again, I do not necessarily disagree. But I feel that this statement is too strong. It reflects the growing influence of people in the pain science (pain neuroscience) camp. I have long believed in the underlying tenets of pain science, and in fact wrote an article advocating the basic principle of pain science a number of years ago, long before it had become so fashionable. And I have long advocated that there is a tremendous lag between structural damage and functional disability (a tenet of pain sciece). But when pendulums swing, they often swing too far. Certainly, we should never rely wholly on an image, for diagnosis, prognosis, or outcome measure. But, having said that, an image can be a very important piece of the diagnostic puzzle. And having this information does not have to be used to scare the patient/client, but rather can be placed in its context when explained to the patient/client.
-
Don’t be worried about rupture.
Pain is protective as it causes unloading of a tendon. In fact most people who rupture a tendon have never had pain and do not present clinically, despite the tendon having substantial pathology.
– Note by Joseph Muscolino. Wow! Even though I agree that it is quite amazing how much structural pathology the body can get away with without any actual pain or even dysfunction, I still would not quite say: “Don’t be worried about rupture.” The word “rupture” implies complete rupture, in other words, complete severance of a structure. A completely ruptured tendon would certainly involve marked dysfunction because the muscle would be unable to transfer its pulling force to its (bony) attachment. If this statement were tempered to say: “Don’t necessarily worry about degeneration.”, I would be fine with it, with the understanding that many people can have moderate to sometimes a marked degree of tissue pathology and still have little or not pain and dysfunction.
-
Don’t Take Short Cuts with Rehabilitation
Taking short cuts with rehabilitation do not work. You need to take the time that the tendon needs to build its strength and capacity. Although this can be a substantial period (up to 3 months or more), the long-term outcomes are good if you do the correct rehabilitation. Short-term treatments can result in a temporary improvement in symptoms, but the pain usually reoccurs when loads are resumed on the tendon.
Conclusion
In summary, exercise-based rehabilitation is the best treatment for tendon pain. A progressive program that starts with a strength program and then progresses through to more spring-like exercises, and endurance aspects will give the right loads on the tendon and the best long-term results.
– Note by Joseph Muscolino: Again, I agree with this statement, but would like to temper it. I strongly believe that strength rehabilitation loading exercises are the key to long-term true and lasting healing of tendon injuries, and all myofascial injuries in fact. But I believe that there is a strong argument to be made for passive manual therapy treatment, especially early on in the healing process of a myofascial injury. Tendon injuries rarely occur in isolation. They are usually accompanied by muscular/myofascial dysfunction as well. And restoring tissue flexibility and joint mobility is often a safer and more effective course to follow before loading exercises are commenced. Or, alternatively, passive manual therapies can accompany active loading exercises during the treatment process to restore tissue flexibility and joint mobility.
This blog post article was created in collaboration with www.terrarosa.com.au.