Self-care for the client/patient with Golfer’s Elbow:
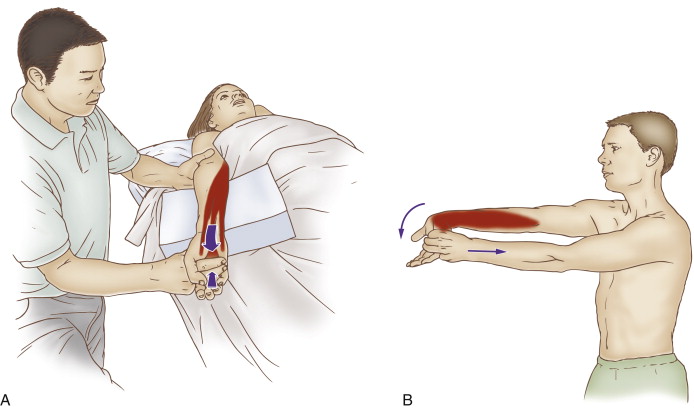
Self-care (and therapist-assisted) stretch for golfer’s elbow. Permission: Joseph E. Muscolino, The Muscle and Bone Palpation Manual, with Trigger Points, Referral Patterns, and Stretching, 2ed. (2016), Elsevier.
Self-care is an extremely important aspect of the treatment for golfer’s elbow. The client/patient should be advised to avoid offending postures and activities as much as possible. Frequent stretching of the hand and fingers into extension should be done (unless tears are present, in which case stretching should be avoided). If inflammation is present, icing should be done. Clients may also choose to take over-the-counter anti-inflammatory medication. If and when signs and symptoms of the condition have resolved, strengthening the forearm/hand musculature should be recommended.
Medical approach to Golfer’s Elbow:
Whenever conservative manual therapy care is not successful, referral to a physician should be considered. Medical management usually involves prescription steroidal anti-inflammatory medication such as cortisone, as well as cortisone injections. If the degenerative phase is present, prolotherapy injections, including platelet rich plasma (PRP) injections are beneficial. Another approach is to “bleed the tendon.” This is done by repeatedly pricking the tendon with a small needle. As with prolotherapy injections, the goal is to stimulate a fibroblastic response to create fascial collagen scar tissue healing of the degenerated and/or torn fascial tendinous tissue. Note: When prolotherapy or bleeding the tendon is employed, the patient/patient must avoid anti-inflammatory medication because it would halt the fibroblastic response and obviate the entire reason for this employing this approach in the first place. In worst-case scenarios, surgery may be done to remove degenerated collagen tissue as well as mend tears.
Manual therapy case study for a client with Golfer’s Elbow:
Edward is a 50-year-old writer. He recently bought a smart phone and has been using it a lot. Because he is right-handed, he holds it in his left hand. A few months after he bought it, he began to feel pain at his left elbow. At first, he didn’t notice that using the phone was aggravating his medial elbow pain, but now he realizes the connection because after holding the phone for more than 10 minutes, his pain increases. He also feels the pain when he is working at the keyboard for a prolonged period of time. And he feels the characteristic pain when lifting heavy objects. Because his elbow pain is interfering with his ability to comfortably work and write at the computer, he decided to go to a clinical orthopedic manual therapist.
The therapist performed active and passive range of motion of the hand at the wrist joint. Active flexion and extension produced pain at the common flexor tendon, as did passive extension; passive flexion was asymptomatic. No pain was elicited with either passive or active radial or ulnar deviation. Palpation at the common flexor belly revealed tightness and marked pain. Palpatory pain was also found at the common flexor tendon and directly on the medial epicondyle of the humerus. The therapist also performed assessment tests for other conditions that could refer pain into the upper extremity and all were found to be negative.
Given the assessment of golfer’s elbow, the therapist recommended two one-hour massages per week, for four to six weeks. Each session consisted of approximately 5 minutes of myofascial spreading, followed by 20-30 minutes of deep tissue work to the left forearm following the golfer’s elbow protocol (presented in Blog #4 on Golfer’s Elbow). The remainder of the time was spent working the rest of Edward’s left upper quadrant with deep tissue work to the hand, posterior forearm, arm and shoulder region; and moist heat, deep tissue work, stretching, and joint mobilization to the upper back, neck, and left upper extremity.
Edward was given self-care instructions including stretching and ice. He was also given recommendations to avoid overuse of his forearm muscles. Specifically, he was told to take frequent breaks when working at the computer, to decrease the use of his cell phone, and when using the phone to hold it in both hands.
At the end of four weeks, Edward’s symptoms had abated approximately 50%. He was now able to function and work, but still had mild/moderate discomfort. The therapist referred Edward to a physiatrist who performed an ultrasound of his left common flexor tendon and found two small tears. Edward opted to have a platelet rich plasma (PRP) injection (instead of deep friction cross fiber work). He resumed orthopedic massage approximately four weeks after the injection. His condition is now 90% resolved with only mild pain if he spends prolonged time in problematic postures. Edward has chosen to continue with orthopedic massage once per week and is considering the possibility of another PRP injection.
Click here for an article on the self-care and medical approaches to tennis elbow.
Note: This is the fifth of five blog post articles on golfer’s elbow.
The five articles are:
- What are the causes of Golfer’s Elbow?
- What are the signs and symptoms of Golfer’s Elbow?
- How do we assess (diagnose) Golfer’s Elbow?
- How do we treat Golfer’s Elbow with manual therapy?
- What are the self-care and medical approaches to Golfer’s Elbow?


