Frozen Shoulder – Introduction:
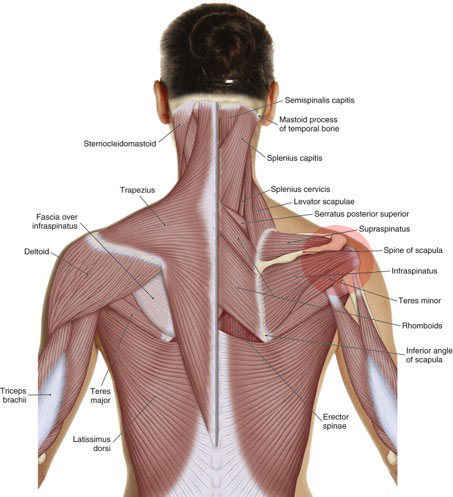
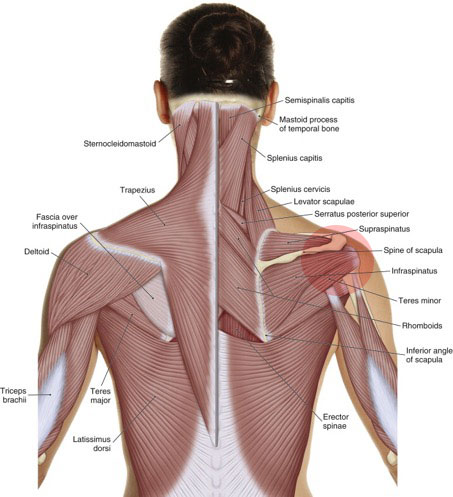
Frozen shoulder involves the rotator cuff musculature. Permission: Joseph E. Muscolino. The Muscle and Bone Palpation Manual: The Skeletal Muscles of the Human Body, 4ed. (2016) Elsevier.
Frozen shoulder is a condition in which the glenohumeral (GH) joint loses mobility, in other words becomes frozen, in one or more ranges of motion. There are two stages to frozen shoulder. The first stage involves contraction of the muscles of the GH joint and is called neurogenic frozen shoulder. The second stage involves the formation of fibrous adhesions and is called adhesive capsulitis. Frozen shoulder rarely occurs by itself; rather it usually occurs in response to another condition of the GH joint.
Causes of frozen shoulder:
The GH joint is often described as a muscular joint. This does not mean that it has more musculature than other joints. It means that proportionally, the GH joint depends more on its musculature for stability because its bony shape and ligament/joint capsule complex are designed for mobility, not stability. The glenoid fossa is a shallow socket and its ligament/joint capsule complex is lax, therefore when stability is needed, contraction of the GH musculature is needed to stabilize the joint.
The most common cause of frozen shoulder is the body’s desire to tighten the musculature, usually the rotator cuff musculature (supraspinatus, infraspinatus, teres minor, subscapularis) around the GH joint after an injury such as a rotator cuff tear or trauma. It is common for musculature around an injured joint to tighten in an attempt to splint/stabilize the joint so that it cannot be moved; the premise being that if the joint cannot be moved/used, it will be rested and have a chance to heal. However, in the case of the GH joint, splinting stabilization of its musculature becomes excessive and often ends up immobilizing/freezing the joint. Often, this response is largely or entirely unnecessary because it occurs after the initial injury is mostly or fully healed.
The first “neurogenic” stage is a response to the injury: muscles are directed to tighten; at this point in time there is no structural component to the frozen shoulder, it is merely a functional response by the nervous system to create muscular hypertonicity. However, the longer the neurogenic stage is allowed to exist, the more fascial fibrous collagen adhesions (“fuzz” in the parlance of Gil Hedley) have a chance to form, beginning the structural “adhesive capsulitis” stage. The progression of frozen shoulder condition is often a vicious cycle: the less the joint is moved, the more adhesions form, further decreasing the joint’s ability to move, allowing for more adhesions to form, etc.
Often, the neurogenic stage is effectively jump started by the client. For example, if post injury or post surgery the arm is placed in a sling for an extended period of time, usually a week or more, the neural pattern of immobilization is initiated, and will more likely become patterned into the nervous system than if the client had not immobilized the arm. It also allows for adhesions to begin forming. Therefore immobilization of the shoulder, or simply not moving it through its ranges of motion, increases the chances that frozen shoulder will occur. For this reason, whenever possible, it is important to avoid immobilization of the GH joint.