Assessment/Diagnosis:
The first key to assessment/diagnosis of a pathologic disc is the clinical presentation. If the condition is severe enough, there will be compression of neural contents. Physical examination orthopedic assessments tests for pathologic discs are done to confirm or rule out the presence of neural compression (nerve impingement).
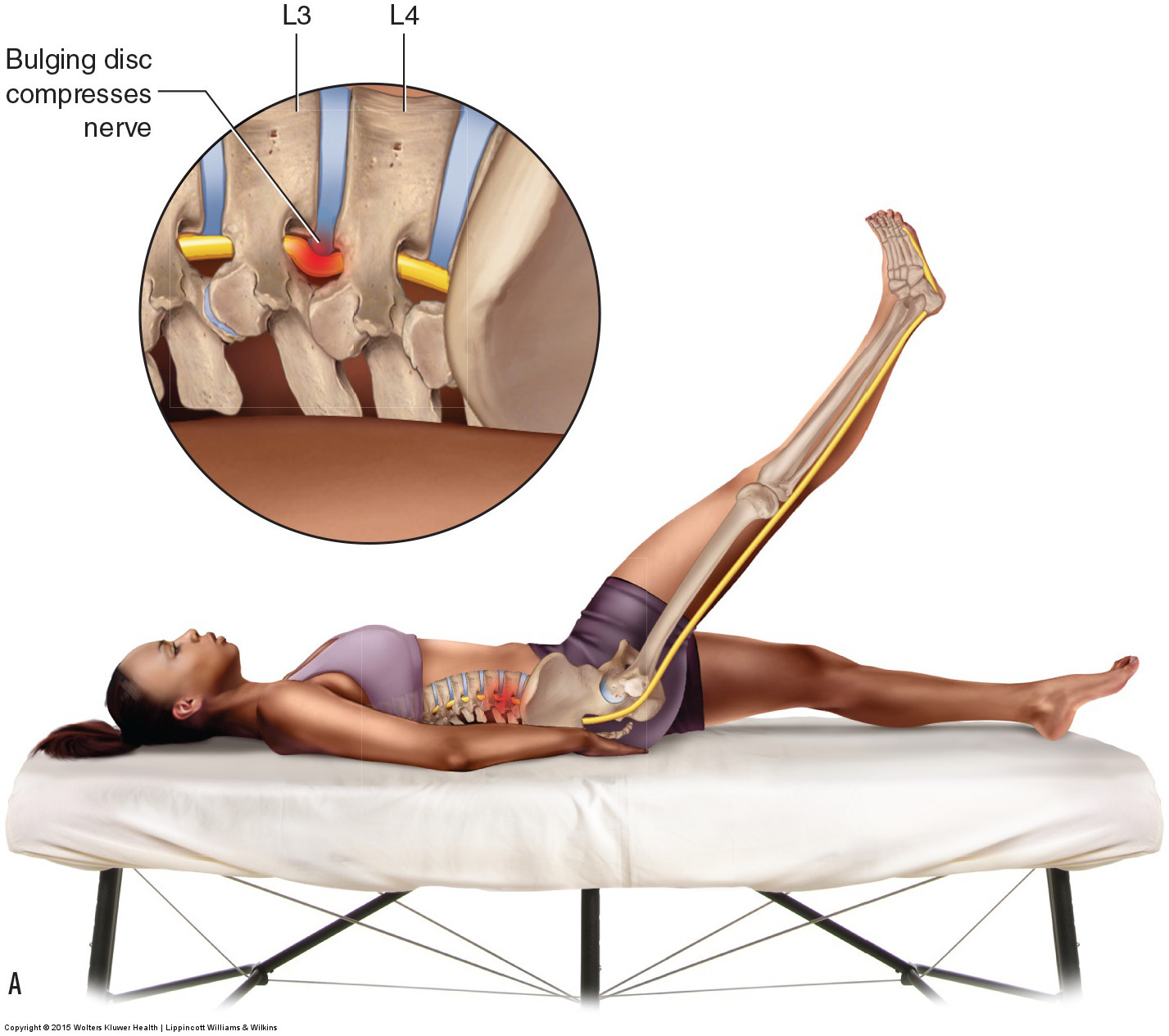
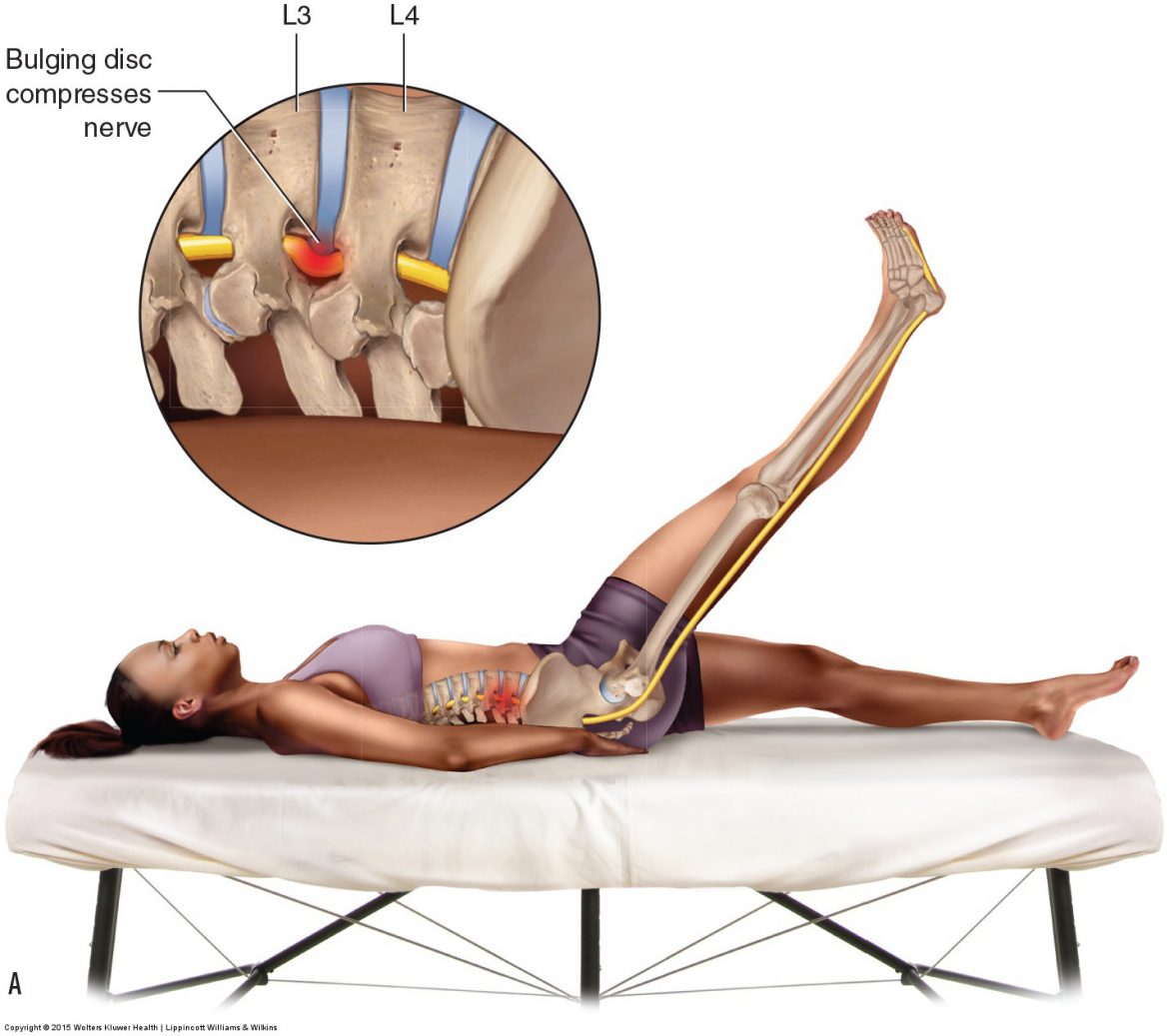
Straight leg raise orthopedic assessment test for a lumbar pathologic disc. Permission: Joseph E. Muscolino. Manual Therapy for the Low Back and Pelvis – A Clinical Orthopedic Approach (2015).
For lumbar disc pathologies, the principle assessment test is straight leg raise (SLR). This can be performed actively or passively, but passive SLR is preferred because it does not involve muscle contraction, which could result in a false positive if there is a muscular strain. As the client’s lower extremity is passively brought into flexion (with the knee joint fully extended), the sciatic nerve is stretched long on the posterior side of the body. If a disc bulge or herniation is taking up space in the intervertebral foramen or central spinal canal (space occupying lesion), then the nerve will be pulled taut against it and symptoms will refer into the lower extremity. To increase the sensitivity of SLR, the tension upon the spinal cord and lumbar nerves can be increased by asking the client/patient to flex their head and neck. Therefore, unlike active and passive SLR tests, which are used to assess strains and sprains, the criterion for a positive SLR test for pathologic disc is referral into the lower extremity (sciatica), not local pain.
The principle assessment test for a cervical pathologic disc is foraminal compression test (also known as Spurling’s test). It is performed by pressing down on the top of the client’s/patient’s head, gradually increasing the pressure; holding this position for a period of 5-10 seconds, and then gradually releasing the pressure. As with SLR test for the lumbar spine, the criterion for a positive foraminal compression test is referral symptomology into the (upper) extremity, not local pain. Foraminal compression test can be followed with maximal foraminal compression test. This is performed by first rotating and laterally flexing the client’s head to one side, and then adding pressure downward. Again, the criterion for a positive test is referral into the upper extremity. The mechanism of these tests is to add compression to the intervertebral foramina (IVFs), so the direction of pressure should be oriented down through the IVFs.
There are three other tests that can be performed that can assess neural compression due to pathologic disc for both the lumbar and cervical regions (as well as the thoracic region). They are slump test, cough test, and Valsalva maneuver. Slump test is performed in steps:
Step 1: The seated client/patient is asked to clasp their hands down behind the back; this increases tension on the brachial plexus of nerves.
Step 2: The client flexes (i.e., slumps) their trunk forward; this increases tension on the entire spinal cord.
Step 3: The client flexes the thigh at the hip joint and extends the leg at the knee joint; this increases tension on the sciatic nerve on that side.
Step 4: The client dorsiflexes the foot at the ankle joint; this further increases tension on the sciatic nerve.
Step 5: (Optional): The therapist can add to the head/neck flexion and/or the ankle joint dorsiflexion.
The slump test is then repeated for the other side lower extremity. If a disc bulge or herniation is compressing upon nervous tissue, symptoms will refer into an extremity.
Cough test is performed, as its name implies, by the client/patient coughing (once or twice) with moderate to strong. The client should not cloud the procedure by using their upper extremity to cover their mouth when coughing because this could possibly cause pain due to the movement of their upper extremity. Valsalva maneuver is performed by asking the seated client to take in a deep breath and then bear down as if at stool in the bathroom, and holding this posture for approximately 5-10 seconds. Because the Valsalva maneuver can possibly create a vasovagal reflex resulting in decreased blood pressure, it is usually recommended that the client is seated during this procedure. Both cough and Valsalva cause increased internal (intrathecal) pressure against spinal nerves. As with all disc assessment tests, referral into an extremity yields a positive finding. Referral into an upper extremity for a cervical disc and referral into a lower extremity for a lumbar disc; and referral into a right-sided extremity for a right-side pathologic disc; and referral into a left-sided extremity for a left-side pathologic disc.
If a client/patient does show sensory symptoms into an extremity, the location of the referral can then be compared to a dermatomal chart to help determine the level of the nerve compression.
Differential assessment:
Any space-occupying condition that causes neural compression can mimic the signs and symptoms of a pathologic disc. These conditions include bone spurs from osteoarthritis (also known as degenerative joint disease), spondylolisthesis, spinal fracture, or tumor. Thoracic outlet syndrome can also cause referral symptoms into the upper extremity. Further, myofascial trigger points in the axial body can refer pain into the extremities, making assessment of a pathologic disc more challenging. Pathologic discs also need to be differentially assessed from local conditions that cause pain within the upper or lower extremities.
It should be noted that the orthopedic assessment test for pathologic disc presented in this chapter will also show positive for any other space-occupying lesion of the IVF or spinal canal, the most common of which is a bone spur causing IVF stenosis (narrowing the space within the foramen). Therefore, technically these tests are not disc tests per se, but rather tests to assess space-occupying lesions.
X-rays can be used to determine the degree of osteoarthritic bone spurring. However, X-rays do not show discs because discs are soft tissue. An X-ray can show the space that a disc occupies, but it does not show the disc itself. Therefore an X-ray can be used to assess the thinning of a degenerated disc, but it cannot determine if a disc is bulging or herniated. Definitive assessment/diagnosis of a disc bulge/herniation is done via MRI or CT-Scan.