Assessment/Diagnosis
In a sense, sciatica is not a condition but rather a sign of another condition: a space-occupying (nerve compression) condition that is compressing the sciatic nerve. Therefore, successful assessment/diagnosis of sciatica depends upon successfully assessing the underlying cause of the sciatic nerve compression.
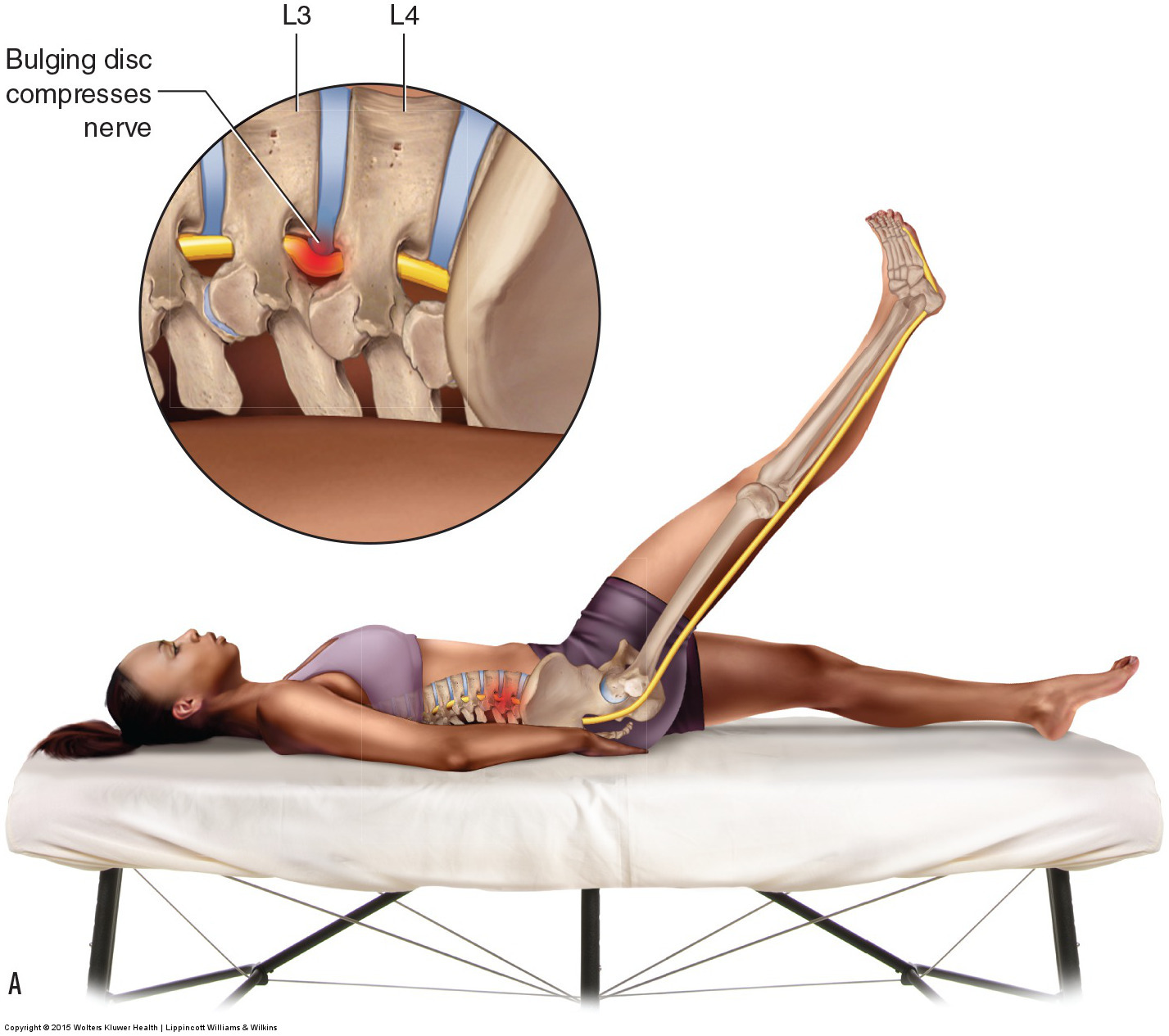
Straight leg raise orthopedic assessment test. Permission: Joseph E. Muscolino. Permission: Joseph E. Muscolino. Manual Therapy for the Low Back and Pelvis (2015).
Physical examination assessment of sciatica begins with straight leg raise (SLR). Straight leg raise is performed by passively raising the lower extremity of the supine client/patient by flexing the thigh at the hip joint with the knee joint extended. This places a tensile force upon all posterior soft tissues, including the sciatic nerve, stretching them longer. If the sciatic nerve is already compressed in the intervertebral foramen (IVF) (or the central canal), then stretching it longer will pull it taut against the space-occupying lesion (bulging/herniated disc or bone spur), thereby increasing the referral symptoms into the lower extremity. For this reason, a positive finding for SLR assessment of sciatica requires referral into the lower extremity. This test would then be repeated for the other side.
Note: Given the mechanism of SLR, active SLR should yield the same results as passive SLR. However, passive SLR removes the need for the client/patient to actively contract their musculature, which might cloud the clinical picture by causing pain due to muscular strain.
Another orthopedic test for sciatica is known as “slump test” because of the slumped posture that the client/patient assumes. This test places tension on the entire spinal cord and peripheral nerves of the upper and lower extremities, therefore it can assess a space-occupying lesion of the cervical and lumbar regions, as well as thoracic outlet syndrome. This test is usually done by performing a number of steps in sequence: The seated client/patient is asked to: 1. clasp their hands behind the back; 2. slump (flex) the thoracic and lumbar spine; 3. flex the head and neck; 4. extend the knee joint and dorsiflex the ankle joint. A positive finding for slump test for sciatica requires referral into the lower extremity. This test would then be repeated for the other side.
Two other orthopedic test for sciatica are cough test and Valsalva maneuver. As its name implies, cough test is performed by asking the client/patient to somewhat forcefully cough. Valsalva maneuver is performed by asking the client/patient to take in a deep breath and hold it in while bearing down as if at stool in the bathroom (note: because Valsalva maneuver can cause a vasovagal reflex that can lower blood pressure, it is usually advised to perform this test with the client/patient seated). The mechanism for both of these assessment tests is to increase intrathecal pressure within the body at the IVFs against the nerve roots. If the underlying compression causing the sciatica is occurring at the IVF, then coughing or straining will likely reproduce or increase referral into the lower extremity. As with SLR and slump test, positive for cough and Valsalva is referral into the lower extremity.
Because sciatica might be caused by piriformis syndrome, it is important to also assess the piriformis for tightness that might compress against the sciatic nerve. This can be done via palpation and by assessing its ability to lengthen by stretching it.

The Sciatic Nerve. Permission Joseph E. Muscolino. Manual therapy for the Low Back and Pelvis – A Clinical Orthopedic Approach (2015)
If the client/patient presents with symptoms of sciatica, it can also be important to assess for muscle weakness that might be due to compression of motor neurons of the sciatic nerve. Asking the client/patient to stand on their heels requires contraction of the dorsiflexors; asking the client/patient to stand on their toes requires contraction of the plantarflexors. Inability to maintain a stance on heels or toes might indicate weakness of the associated musculature due to motor neuron compression (of course, it might simply indicate poor balance).
Note: A physician has a number of testing procedures that can be ordered to diagnose the cause of sciatica. These include X-Ray to assess osteoarthritic bone spur encroachment in the IVFs, MRI or CT Scan to assess pathologic disc or other soft tissue encroachment in the IVF or central canal, and electrophysiologic testing in which conduction of the sciatic nerve is directly assessed.
Differential assessment
Sciatica causes symptoms into the sciatic nerve distribution in the lower extremity. Therefore, any condition that causes symptoms into this region could potentially be mistaken for sciatica. Many conditions can do this. Foremost amongst these is myofascial trigger point referral or referral from an irritated sacroiliac joint. Therefore, before being confident in the assessment of sciatica, it is important to rule out these other conditions. Local pain in the lower extremity caused by tight musculature, sprains, and strains, might also be mistaken for sciatica. And because sciatica can cause numbness into the foot, diabetes and other conditions that cause peripheral neuropathy must also be differentially assessed.
Other nerve compression syndromes might also be mistakenly assessed as sciatica. Compression of the posterior femoral cutaneous nerve, which exits through the greater sciatic foramen directly next to the sciatic nerve, can also cause sensory paresthesia into the posterior thigh. Compression of the lateral femoral cutaneous nerve can cause referral symptoms into the anterolateral thigh; this condition is called meralgia paresthetica. Compression of the femoral nerve can cause paresthesia into the anterior thigh and leg. And compression of the obturator nerve can cause paresthesia into the medial thigh.


