Note: This is the eighth blog post article in a series of 14 articles on Assessment/Diagnosis of musculoskeletal conditions of the neck (cervical spine). See below for the other articles in this series.
Foraminal Compression (Spurling) Test
The foraminal compression test, also known as Spurling test, is used to assess/diagnose a space occupying condition of the cervical spine.
As its name implies, the test involves compressing the intervertebral foramina (IVFs) of the cervical spine. The therapist performs this test by placing the hands with fingers overlapped or interlaced on the top of the client’s head and then slowly and evenly directing gentle and then moderate pressure downward. The compression is usually held for approximately 5 to 10 seconds and then slowly released.
- Note: the term “space occupying condition (lesion)” is essentially used to describe a condition in which there is compression on a spinal nerve in the intervertebral foramen (IVF) (or perhaps the spinal cord in the spinal canal).
- In other words, the condition/lesion involves space that is needed by the nerve being occupied by some other structure, thereby compressing/pinching the nerve.
- Most often, a space occupying condition is caused by a pathologic disc (bulging or herniated/ruptured/prolapsed), a bone spur of osteoarthritis (degenerative joint disease), or perhaps swelling or ligament hypertrophy.
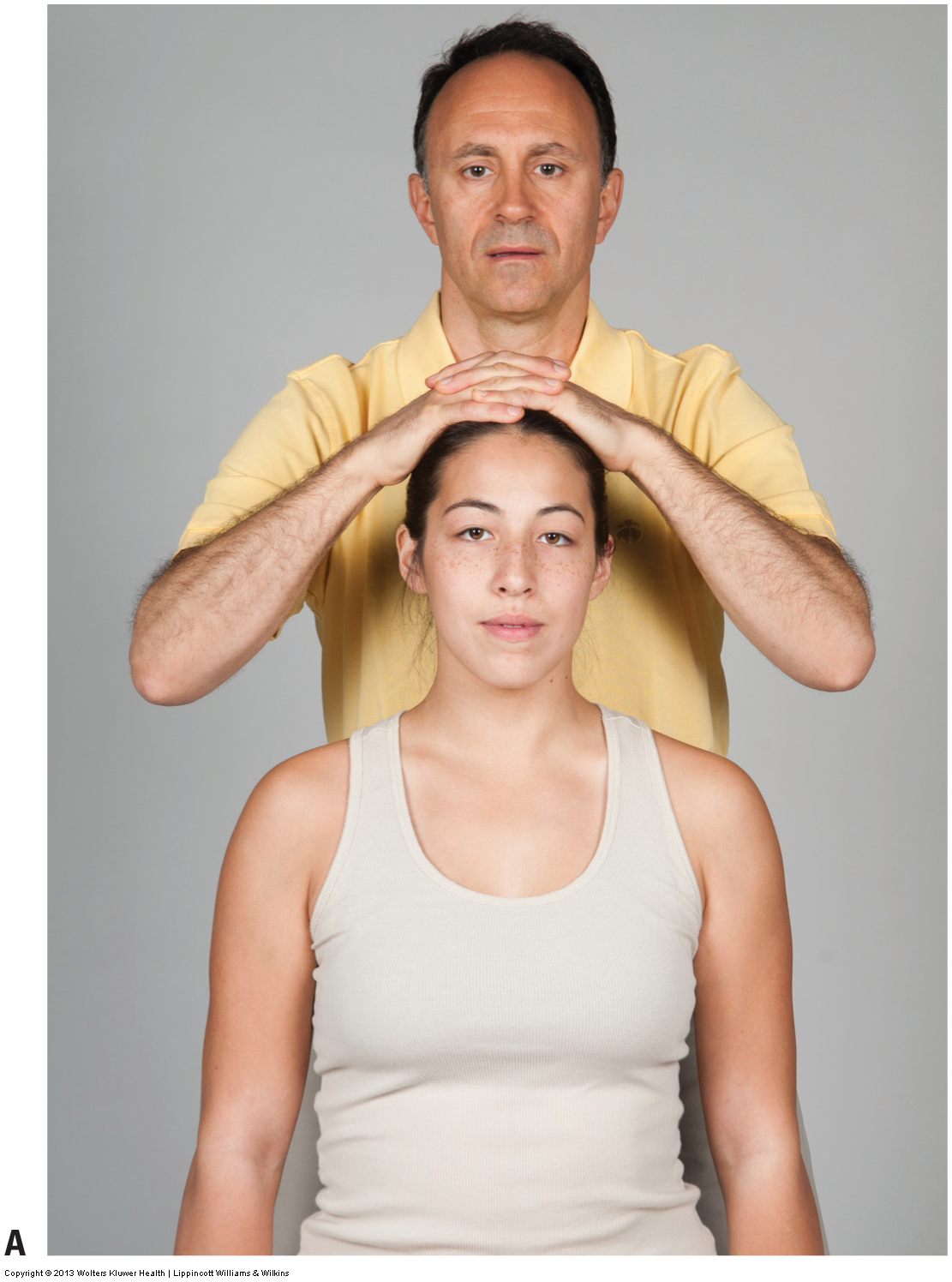
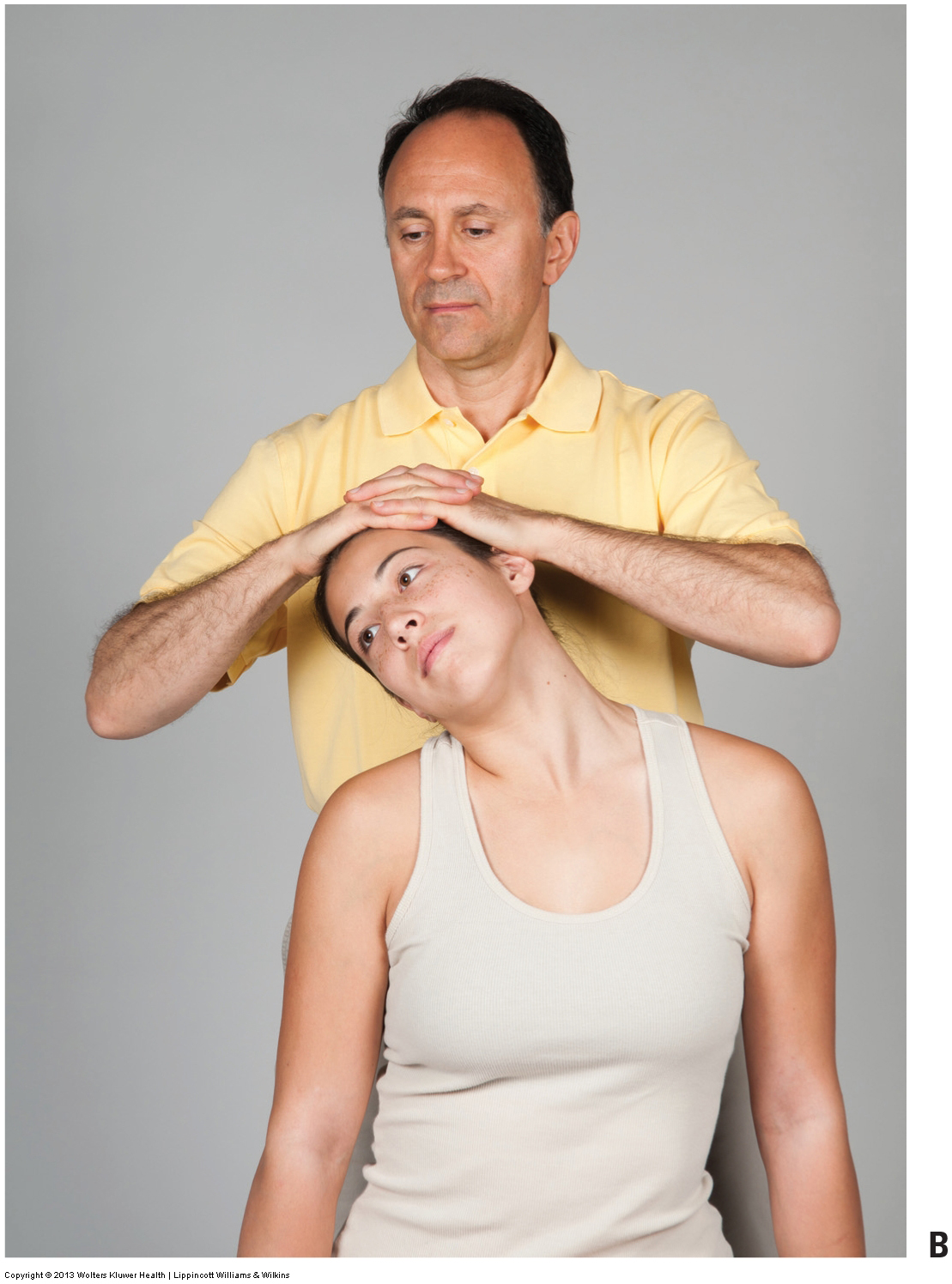
Figure 6. Foraminal compression test to assess for a space occupying condition of the cervical spine. (A) The therapist places downward pressure on the client’s head while the client’s neck and head are in a neutral position. (B) Maximal foraminal compression test to the right side of the client’s body. Pressure can either be directly downward or downward and slightly posteriorly and laterally. Courtesy Joseph E. Muscolino.
Foraminal compression test may be performed with the client’s head in different positions.
- First, the test is performed with the client’s head in neutral position (Fig. 6A). The pressure should be directed directly downward.
- To increase the compression and therefore the sensitivity of the assessment procedure, the test can be repeated with the client’s head extended, laterally flexed to the side, and rotated to the same side (the lateral flexion and rotation should be to the side that is suspected of having the space-occupying lesion).Performing the test in this position is often referred to as maximal foraminal compression. Pressure can be directed downward or even slightly posteriorly and laterally to the side that the client laterally flexes (Fig. 6B).
- Adding these positional components increases the foraminal compression on one side but decreases it on the other side, so the maximal foraminal compression test needs to be repeated on the other side of the client’s body. Given the vulnerability of this position, it is extremely important that the force downward is applied gently at first and only increased to moderate pressure at most as you feel for the tissue tension barrier of the client’s neck.
- Compressing the intervertebral foramina diminishes the space for the spinal nerves that enter/exit the spinal cord. If the client is already experiencing compression of a cervical spinal nerve as a result of one of the space-occupying lesions mentioned previously, then further compression of the spinal nerve with this test may reproduce or increase these symptoms. Most often, they manifest as some form of sensory disturbance referring down into the upper extremity. For example, the client may feel shooting or burning pain, tingling, or numbness into the arm, forearm, and/or hand. A healthy client will have a negative test result.
- Referral symptoms into the upper extremity qualify the foraminal compression test as positive; the side to which the symptoms refer is the side where the space-occupying lesion exists. The presence of neck pain or discomfort is not considered positive because most neck conditions will produce some neck pain or discomfort when the cervical spine is compressed. A positive foraminal compression test indicates a space-occupying lesion, most commonly the presence of a pathologic disc or moderate to severe DJD (osteoarthritis). A negative foraminal compression test indicates the absence of moderate to severe DJD and the absence of a pathologic disc, or at least the absence of a moderate to markedly damaged disc. (A mildly bulging or herniated disc may produce a negative test result, especially if only the mild version of the assessment procedure is performed.)
- Note: Given that clients may present with different postures to their neck, when in doubt as to the direction that you need to press, keep in mind that the mechanism of this test is to place the compression force through the IVFs. So put on your X-ray glasses and picture the location of the IVFs and direct your pressure through them. BTW, X-ray glasses are an automatic part of your anatomy when you really learn well and know the anatomy of the human body!
Positive Foraminal Compression Test
- A client who is found to have a positive foraminal compression test result should see a physician. If the client is not already consulting a physician for this condition, then the therapist should provide a referral.
- The therapist can continue to treat this client, but it is important to avoid using any manual pressure and positioning of the client that could increase symptoms into the upper extremity.
Cough Test and Valsalva Maneuver
- Both the cough test and Valsalva maneuver/test are designed to increase intrathecal pressure, or pressure on the spinal cord and pressure on the spinal nerves in the intervertebral foraminal spaces (i.e., to assess a space occupying condition).
- The mechanics are the same as with the foraminal compression test: increased compression on these neural structures can cause referral of symptoms into the upper extremity in a client with a space-occupying lesion.
- However, whereas the foraminal compression test only increases compression to the cervical spine (and perhaps the upper thoracic spine), the cough test and Valsalva maneuver cause increased compression to be experienced throughout the entire spine. Therefore, they will also assess a pathologic disc and advanced osteoarthritis (OA) / degenerative joint disease (DJD) of the lumbar spine (if the client experiences referral symptoms into the lower extremity).


Figure 7. Cough test and Valsalva maneuver to assess a space occupying condition. (A) In the cough test, the client is asked to cough forcefully. (B) In the Valsalva maneuver, the client is asked to inhale a deep breath and hold it, and then bear down as if moving the bowels. Courtesy Joseph E. Muscolino.
- The cough test is performed by asking the seated client to forcefully cough (Fig. 7A).
- The Valsalva maneuver is performed by asking the seated client to take in a deep breath, hold it in, and bear down as if moving the bowels (Fig. 7B). To preserve client modesty and avoid possible embarrassment, avoid eye contact with the client when the Valsalva maneuver is being performed. In each case, as with the foraminal compression test, local pain in the neck is not a positive sign. A positive sign is the presence of referral symptoms into the upper extremity (or lower extremity for a lumbar spine space-occupying lesion).
- Note: Performing the Valsalva maneuver can result in a temporary decrease in blood flow to the heart and brain, possibly causing the client to become dizzy and perhaps even faint (vasovagal response/syncope). Completing the maneuver also causes a sudden increase in blood flow to the heart. This can cause an increased strain on the heart and may be risky for clients who have a weak heart (as from congestive heart failure or other advanced cardiac disease). Given that the client could become dizzy and/or faint, it is important to perform the Valsalva maneuver with the client seated (not standing).
Cervical Distraction Test
- The (cervical) distraction test, like the foraminal compression test, is performed to assess a space occupying condition of the cervical spine; however, it is performed in a manner that is effectively the opposite of the foraminal compression test. Whereas the foraminal compression test compresses the intervertebral foramina by means of the therapist’s pressing down on the client’s head, the distraction test decompresses (distracts/tractions) the cervical spine by means of the therapist’s lifting it.
- To perform this test, the client is seated and the therapist places their thenar eminences inferior to the mastoid processes of the temporal bones, and then lifts the client’s head superiorly, thereby tractioning the cervicocranial region (head/neck) and opening up the intervertebral foramina (Fig. 8A).
- The client may be supine instead (Fig. 8B).
- Note: Be careful not to squish the client’s ears.
- Further note: Some therapists perform this test by contacting the client’s mandible. However, be aware that contacting the mandible will put considerable force through the client’s temporomandibular joints (TMJs), which is either precautioned against or contraindicated.
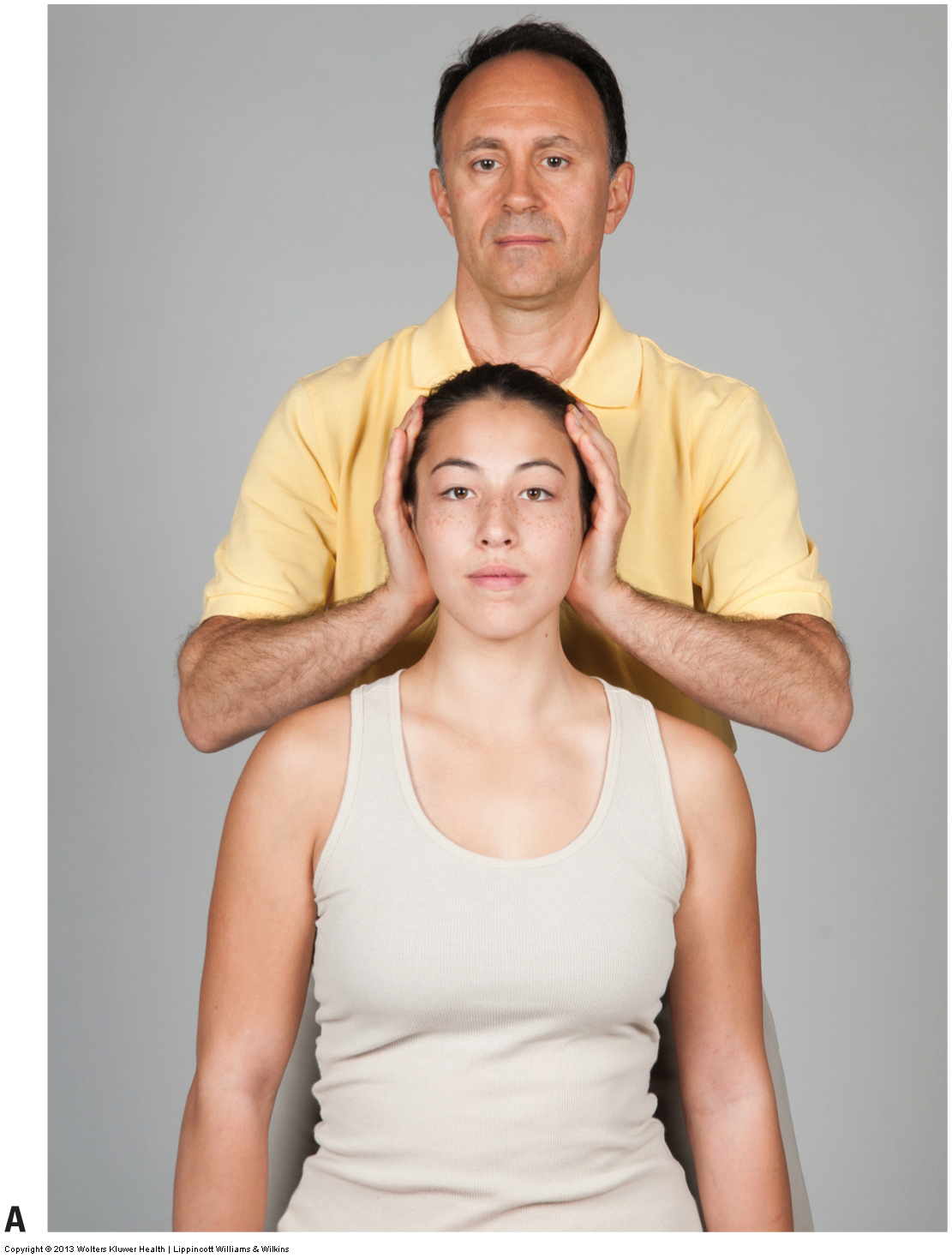

Figure 8. Distraction test for the cervical spine to assess a space occupying condition. (A) The therapist lifts up on the client’s occiput and forehead/parietal region, distracting/tractioning the cervical spine and opening up the intervertebral foramina. (B) The distraction test with the client supine. Courtesy Joseph E. Muscolino.
- For the cervical distraction test, a positive finding occurs if the client’s upper extremity sensory referral symptoms are relieved or decreased.
- The distraction test will be positive for a client with a space-occupying lesion such as a pathologic disc or advanced OA/DJD that compresses the spinal nerves in the intervertebral foramina.
- The reasoning behind the test is that if decreasing the amount of compression on the spinal nerves also decreases the client’s symptoms, then the spinal nerve compression from the space-occupying lesion must be the cause of the symptoms.
- Note: Given that a decrease in the degree of upper extremity referral is the criterion by which cervical distraction test is considered to be positive, there is no reason to perform this test test unless the client is experiencing upper extremity referral symptoms at that exact moment.
This blog post article is the eighth in a series of 14 blog post articles on Assessment/Diagnosis of musculoskeletal (neuro-myo-fascio-skeletal) conditions of the neck (cervical spine).
The articles in this series are:
- Introduction to Assessment/Diagnosis of the Neck
- Verbal and Written Health History
- Overview of Physical Examination Assessment
- Postural Assessment
- Neck General Orthopedic Assessment: Range of Motion and Manual Resistance
- Palpation Assessment
- Motion Palpation (Joint Play) Assessment
- Special Orthopedic Assessment Tests for the Neck – Space Occupying Conditions
- Special Orthopedic Assessment Tests – Space Occupying Conditions – Slump Test
- Orthopedic Assessment of Thoracic Outlet Syndrome – Adson’s, Eden’s, Wright’s
- Orthopedic Assessment of Thoracic Outlet Syndrome – Brachial Plexus Tension Test
- Special Orthopedic Assessment Tests – Vertebral Artery Competency Test
- Treatment Strategy and Treatment Techniques
- Assessment and Treatment of Specific Musculoskeletal Conditions


