Manual therapy treatment
Assuming that the whiplash injury resulted in a strain and/or sprain, treatment can differ depending on the condition and on the stage of the condition.
Acute stage – strains and sprains: For both strains and sprains, when in the acute stage, ice should be used for the swelling. Gentle effleurage can be helpful toward dispelling inflammation.
Chronic stage – strain: In the chronic stage, massage and other manual therapy treatment for a strain is principally geared toward relieving muscle tension and adhesions in the bellies of the affected musculature. Most any massage stroke can be used for muscle strains: however, a good protocol to follow is to begin with longitudinal stripping strokes along the length of the muscle. Pressure should begin light and gradually transition to deep pressure as the work progresses. Be sure to work into the deeper transversospinalis musculature within the laminar groove. Cross fiber work should then be done for the entire length of these muscles, but should be especially concentrated near their superior attachment sites.
Stretching is also beneficial. Stretching the neck into flexion stretches the posterior neck musculature. Lateral flexion can be added to the flexion to focus the stretch to the opposite side of the neck. If both sides of the neck were injured, then the stretch should be performed sequentially, first with lateral flexion to one side and then with lateral flexion to the other side. Rotation can also be added to focus the stretch to specific muscles in the back of the neck. Stretching is always more effective when performed after the patient’s/client’s tissues are first warmed up. Therefore moist heat before stretching is beneficial.
If anterior neck muscles were injured and need to be stretched, then the patient’s/client’s neck needs to be stretched posteriorly into extension. This should be done with caution (before stretching the neck into extension, it is recommended to first perform vertebral artery competency test). As with stretches for the back of the neck, lateral flexion and/or rotation can be added to focus the stretch to one side of the anterior neck.
Grave IV joint mobilization (arthrofascial stretching) for the lower cervical spine. Permission: Joseph E. Muscolino. Advanced Treatment Techniques for the Manual Therapist: Neck (2013).
Chronic stage – sprain: A neck sprain is more problematic to treat because it involves overstretching of ligaments, which causes joint instability. This is challenging to treat because soft tissue manipulation is effective at making tight/taut tissue looser, not making lax tissue tauter. Massage can be done to the region to loosen tight musculature and to prevent excessive fascial adhesions from developing, but even here, caution is advised because muscle tightness and the development of fascial adhesions may aid in increasing stability to the region. Having said this, muscular spasming as a result of any injury, including whiplash, is often excessive and the pain from the tight musculature becomes more problematic for the client than the actual whiplash injury itself. So addressing tight myofascial tissue is usually extremely important with clients/patients who have a chronic whiplash injury. Also, working into musculature can indirectly improve joint instability if so doing improves muscular functioning to help stabilize the spinal joints). A good approach to follow is to massage the client/patient with the goal of reducing any muscle spasming that is present, but if the patient’s/client’s neck continually tightens back up (after perhaps a few weeks or a month or so of treatment), perhaps that degree of muscle splinting is necessary to stabilize the neck due to the weakened ligaments. For this determination to be accurate, care should have been administered at least twice per week. (Note: If this necessary “splinting” is found, then strengthening the musculature is indicated.)
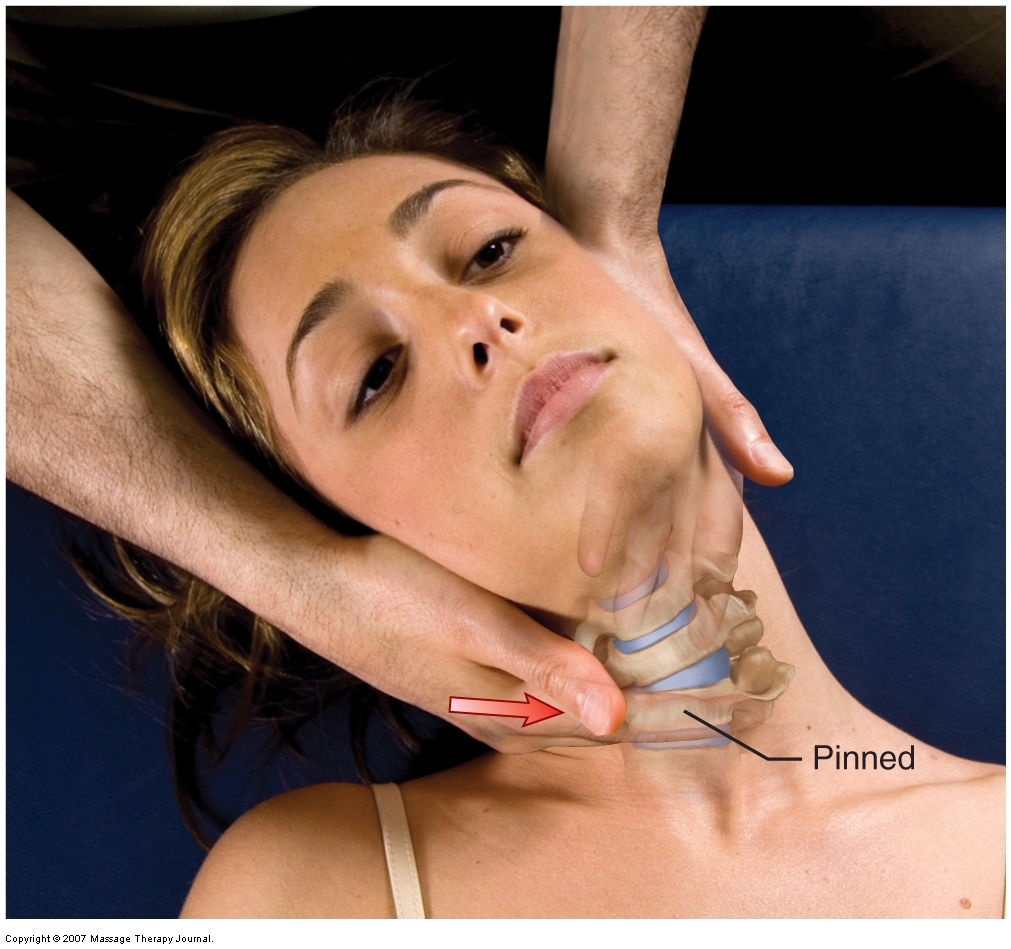
Joint instability often results in hypomobile joint dysfunction as a compensation for the joint hypermobilities. In these cases, it is important to perform joint mobilization (arthrofascial stretching) to loosen any hypomobilities that are present; this is especially important for chronic whiplash injuries. If the principal aspect of the patient’s/client’s injury is instability due to ligament sprain of the neck, then recommending strengthening of the musculature is extremely important.
Summary of Manual Treatment Protocol for Acute Whiplash
| 1. Ice |
| 2. Gentle soft tissue manipulation (effleurage) to the neck and upper back |
Summary of Manual Treatment Protocol for Chronic Whiplash
| 1. Soft tissue manipulation to the neck muscles: begin with light pressure and transition to deeper pressure. Be sure to work the deeper laminar groove transversospinalis musculature. |
| 2. Moist heat followed by stretching to the neck |
| 3. Joint mobilization as appropriate |
| 4. Sprain: Recommend strengthening |
Precautions/contraindications
When working on a client/patient who has experienced a whiplash injury, be sure that the client/patient does not have anything more serious such as a disc pathology or fracture. Stretching the neck should be performed with caution if the client’s/patient’s cervical spine is unstable due to a ligament sprain. If the client’s/patient’s neck is being stretched posteriorly into extension, perform this stretch with caution because many client/patients, especially elderly client/patients, cannot tolerate having their head and neck brought back into extension. If a disc pathology is present, lateral flexion to that side is also contraindicated.


