Manual therapy treatment:
Manual therapy treatment for spasmed muscles of the neck (tightness of neck musculature) includes all the major soft tissue technique tools. Heat hydrotherapy, soft tissue manipulation, stretching, and joint mobilization (also known as arthrofascial stretching/AFS). It is generally advisable to begin with techniques that warm the tissues such as heat and/or soft tissue manipulation. Stretching should always be done after the tissues are warmed. Although joint mobilization is not directly a technique approach for tight musculature, given that tight musculature will restrict joint motion and joint dysfunction can lead to tight musculature, it is a good idea to include joint mobilization in the treatment approach. (Note: If a joint dysfunction hypomobility is limiting your ability to stretch the neck, it is usually advisable to first mobilize the neck joints and then perform stretching.)
When working on a client who has tight neck musculature, the specific manual therapy soft tissue strokes that should be employed will vary based on which muscles need to be treated. However, it is always a good idea to treat the entire tight muscle, from attachment to attachment. If deeper muscles are tight, deep pressure (within the client/patient’s tolerance) is often optimal. Although the posterior neck can be treated with the client/patient prone or side-lying, supine position often allows for the best body mechanics, and therefore the most pressure with the least effort. To best access the laminar groove musculature (the largest muscle of the posterior neck, the semispinalis of the transversospinalis group is located here), passively rotate the client/patient’s neck approximately 45 degrees to the opposite side. For proper body mechanics, when creating the pressure, be sure to keep your elbow in against your core (or as close as possible) and generate the force from your core. I like to say that your elbow should be inside your anterior superior iliac spine (ASIS). It would actually be a bit higher than the ASIS, but this is a good way to visualize the elbow placement.
If manual therapy deep pressure is performed with the client/patient prone, when working on the lower to middle neck, pressure should be directed anteriorly (down toward the floor). But when working the upper neck/suboccipital region, be sure to change the direction of the pressure to be more superior/cephalad in orientation. If there is trigger point referral into the upper extremity, it is generally a good idea to work the region(s) of upper extremity referral after working the neck itself.
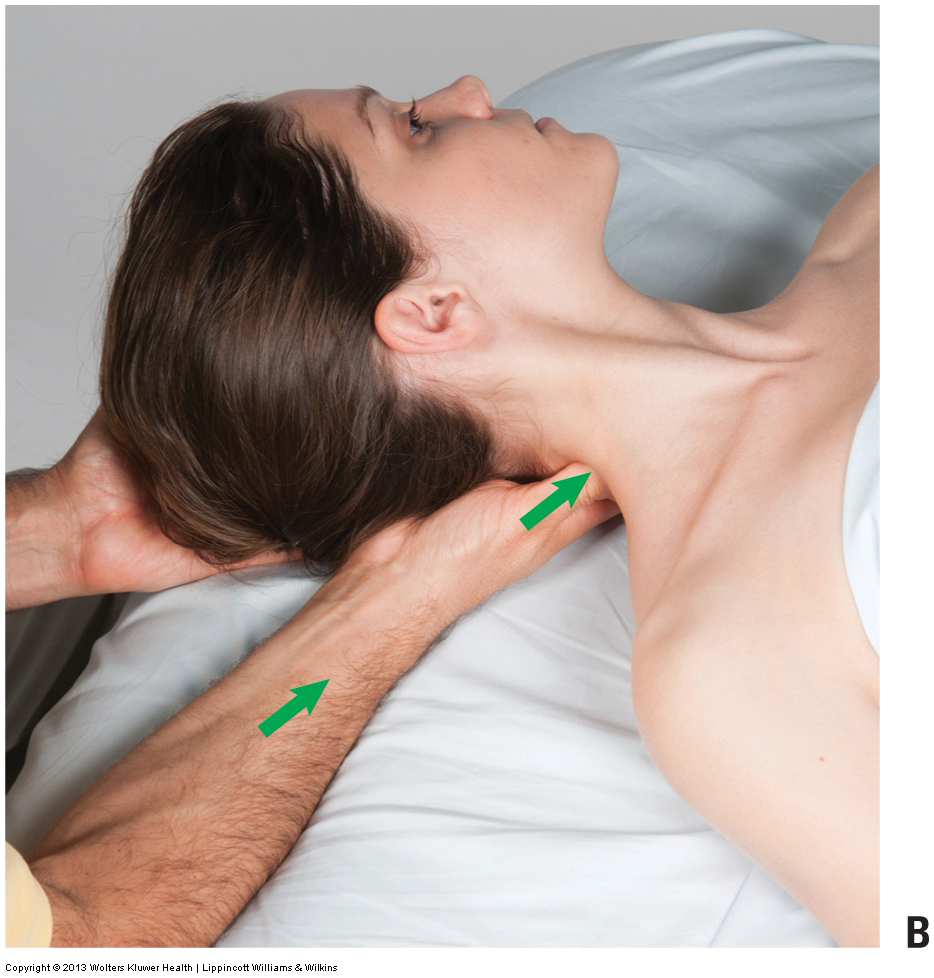
Using the core to generate deep pressure massage into the neck. Permission: Joseph E. Muscolino. Advanced Treatment Techniques for the Manual Therapist: Neck (2013).
With all manual therapy deep pressure into the spasmed muscles of the neck, but especially with side-lying work, be sure to stay posterior to the transverse processes of the spine (try and stay more posterior over the laminar groove musculature). The transverse processes are pointy and superficial immediately deep to the skin and would be painful if contacted by the therapist with deeper pressure. Having the client/patient slightly rotate away so that the posterior laminar groove region is oriented toward the ceiling facilitates working this area when doing side-lying work.
Once the neck as been warmed up, it can be stretched. Manual therapy stretching of the posterior compartment involves flexion of the neck. To focus the stretch to one side posterior quadrant, opposite-side lateral flexion should be added. Rotation to either side can be added in to further focus the stretch to certain muscles. For example, stretching the neck into flexion, left lateral flexion, and right rotation will optimally stretch the right upper trapezius; whereas stretching the neck into flexion, left lateral flexion, and left rotation will optimally stretch the right splenius capitis and cervicis.
Given that joint dysfunction is often a cause or a consequence of tight cervical musculature, it is important to perform manual therapy joint mobilization (arthrofascial stretching) for any hypomobile joints that are found in the cervical spine.
Note: It is usually best to stretch the neck after massage is done. However, if very deep pressure is done, then it might be preferable to stretch (and perform joint mobilization) before doing the deep work because very deep work sometimes causes the client/patient to guard, making it more difficult to stretch the client/patient’s neck.
Summary of Manual Treatment Protocol for Tight Musculature of the Posterior Neck
| 1. Heat |
| 2. Soft tissue manipulation |
| 3. Stretching |
| 4. Joint mobilization |
| 5. Soft tissue manipulation into the upper extremity if trigger point referral is present |
| 6. Self-care: Moist heat followed by stretching |
Note: If the client’s neck tightness is being caused by a hyperkyphotic thoracic postural distortion pattern, usually as part of upper crossed syndrome, then it is essential to perform manual therapy to the thoracic spine as well. Soft tissue manipulation and joint mobilization (arthrofascial stretching/AFS) as well as strengthening of the weak/inhibited musculature of upper crossed syndrome is essential.
Precautions/contraindications:
Deep manual therapy work into the client/patient’s posterior neck should always be done within the client/patient’s tolerance. If the anterior neck is tight, be sure to first inform the client/patient and obtain verbal consent before massaging this region because many client/patients are very sensitive and guarded in the front of their neck. Stretching and joint mobilization might be contraindicated if the client/patient has a pathologic disc. As a rule, avoid stretching the client/patient’s neck into extension or lateral flexion to the side of disc pathology. Further, before stretching the patient’s/client’s neck into extension, the vertebral artery competency test should be done.


