Hypertonic musculature, or tight musculature is an important condition to discuss for two reasons:
- Tight musculature is the most common presenting complaint that a manual/movement therapist will confront.
- Tight musculature is usually a component of every other musculoskeletal condition of the neck.
Of further significance is the fact that tight musculature is so often ignored by conventional medical professions. There are medical specialties for every organ system of the body, but there is no “muscle doctor.” Even the chiropractic profession usually relegates the importance of tight musculature to a position of lesser importance compared with joint positioning and function. Perhaps the importance of tight musculature is overlooked because it does not show on x-rays, other radiographic imaging, or in laboratory results. For this reason, manual therapists who are highly trained in myofascial/muscle palpation assessment skills and soft tissue treatment techniques have the opportunity to step into this niche.
Description of Hypertonic Musculature
A hypertonic muscle is one that has too much tone; “hyper” denotes an excessive amount. Tone refers to tension; in other words, it is the pulling force of a muscle. And the concept of a hypertonic muscle is usually thought of when the muscle is at rest, in other words, at its baseline tone. The degree of tone that a muscle has varies based on the degree of its contraction.
There are two types of hypertonic musculature:
- a globally tight muscle
- a myofascial trigger point (TrP)
The first term is used to describe an entire muscle or large portion of a muscle that is too tight; the second term is used to describe a small focal area of muscle tightness that can refer pain to a distant site.
GLOBALLY TIGHT MUSCULATURE:
When we consciously contract a muscle, its tone is high. However, when a muscle is at rest and we are not consciously directing it to contract, other than a small amount of baseline tone to maintain the posture of the joint, it should be relaxed. This condition is called resting tone. A resting tone greater than the amount needed to maintain joint posture is what defines a muscle as being hypertonic. Other terms often used synonymously are spasm, cramp, and contracture, all of which essentially describe a muscle whose baseline tone is excessive or hypertonic.
Mechanism of Globally Tight Musculature
The physiologic mechanism of a globally tight muscle is determined by muscle spindle fibers (also known as spindle fibers, spindle cells, or intrafusal fibers – note: regular muscle fibers are known as extrafusal fibers). Muscle spindle fibers are located within the belly of a muscle and lie parallel to the regular fibers of the muscle. Similar to these regular muscle fibers, spindle fibers have the ability to contract and relax. But they also possess another feature that regular muscle fibers do not. Muscle spindles are receptor cells that have the ability to detect when they are being stretched. They are sensitive to both how quickly and how far they are stretched. The sensitivity of their setting is determined by the gamma motor system of the brain, which can order them to contract and tighten, or allow them to be relaxed and loose. The tighter the muscle spindles are set, the more sensitive they are to stretch; the looser they are, the more tolerant they are to being stretched.
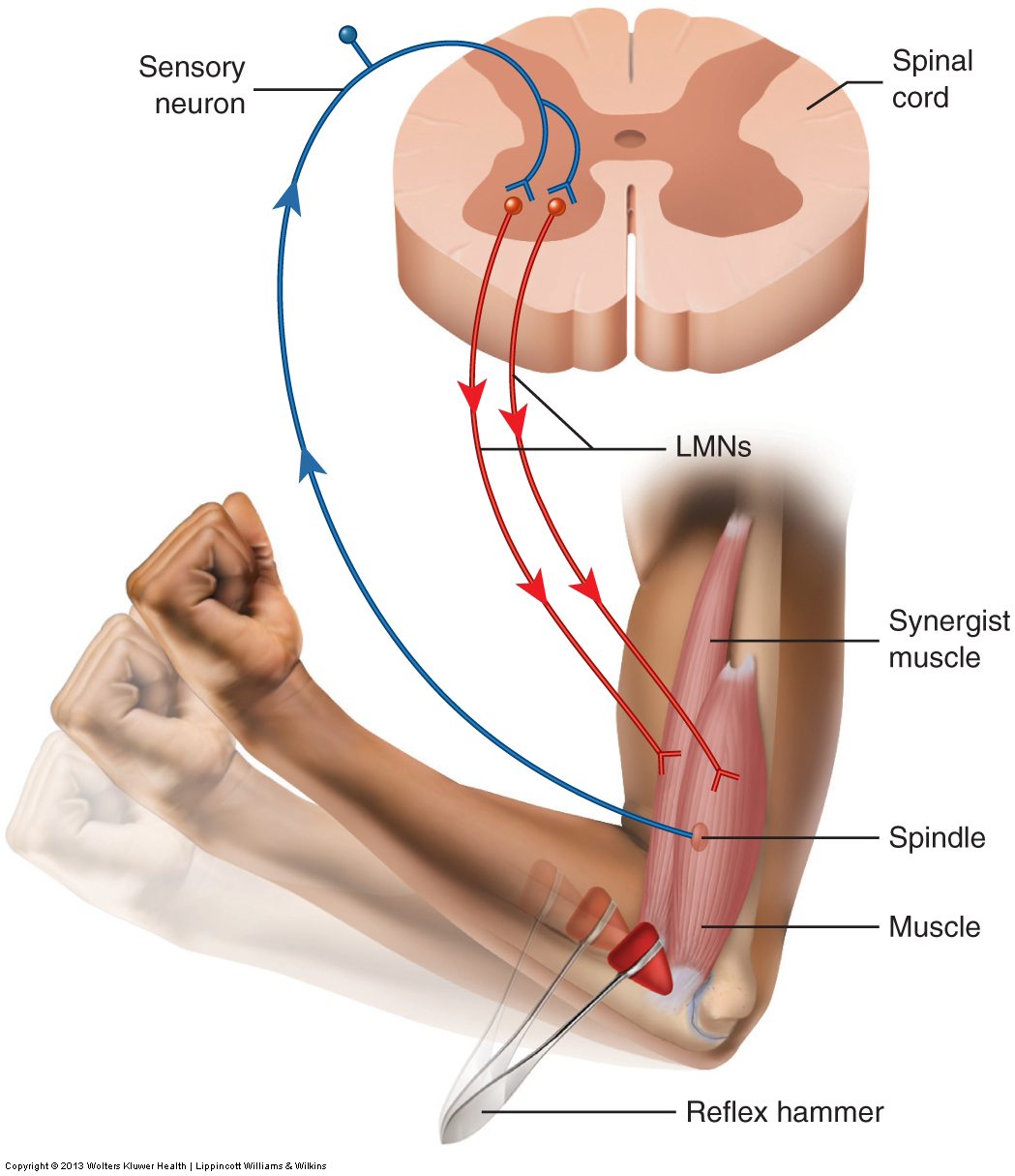
If a muscle is stretched, all of the fibers within the muscle, both regular and spindle, are lengthened. If this stretch occurs quickly or is farther than the spindle fibers can comfortably allow, they sends a signal via sensory neurons into the spinal cord. These sensory neurons then synapse with lower motor neurons that return to the muscle, ordering the regular (extrafusal) fibers of the muscle to contract (Fig. 2). This is called the muscle spindle reflex, or stretch reflex, and is protective in nature. By tightening the muscle, the stretch is stopped and the muscle is protected from being overstretched and perhaps torn.
The stretch reflex is usually only thought of as protecting a muscle from strong forces such as whiplash accidents. However, the stretch reflex is also responsible for setting resting tone of the musculature. When the gamma motor nervous system directs the spindle fibers within a muscle to contract, they shorten. Then when the person moves, as soon as that muscle is stretched even a small amount more than the length of its spindles, the stretch reflex will cause the muscle’s fibers to contract to the tension level set for the spindles. In this manner, the length of a muscle’s fibers, or its tone, will match the length and tone set for its spindles. The term muscle memory is often used to describe this baseline tone of a muscle. Muscle memory resides in the nervous system, not in the muscle itself.
Note: What is Torticollis?
A specific type of hypertonic neck problem that occurs with some frequency is called torticollis (also known as wry neck). Torticollis is primarily the result of a spasm of the sternocleidomastoid muscle and/or the trapezius muscle on the same side. The result is that the client’s head and neck are flexed laterally to one side and rotated to the other side (“torti” means twisted; “collis” means neck). This condition may occur suddenly, often as a result of overuse and/or poor sleeping postures. As with any condition that involves muscular spasms, manual and movement therapy treatment techniques can be very effective.
Causes of Globally Tight Musculature
There are a number of causes for globally tight musculature of the neck. Four of the most common causes are as follows:
- Muscle Overuse
- Muscle Splinting
- Muscle Adaptive shortening
- Muscle Overstretching
In each case, the muscle memory tone set by the gamma motor system and muscle’s stretch reflex is increased. Although this chapter addresses each cause separately, when a client presents clinically with tight musculature, the mechanisms of the causes can and often do overlap.
- Muscle Overuse
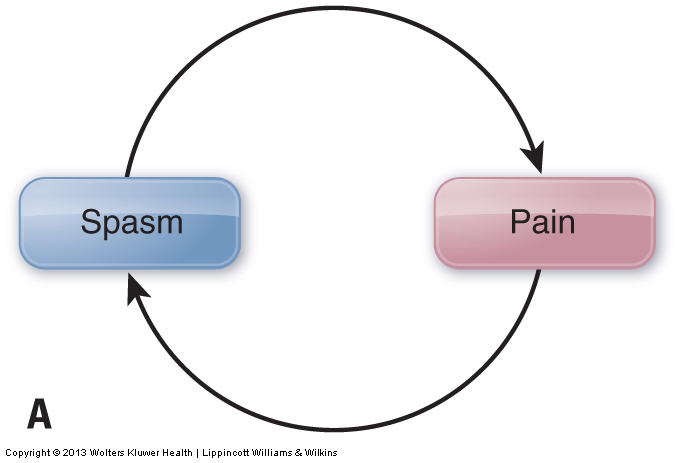
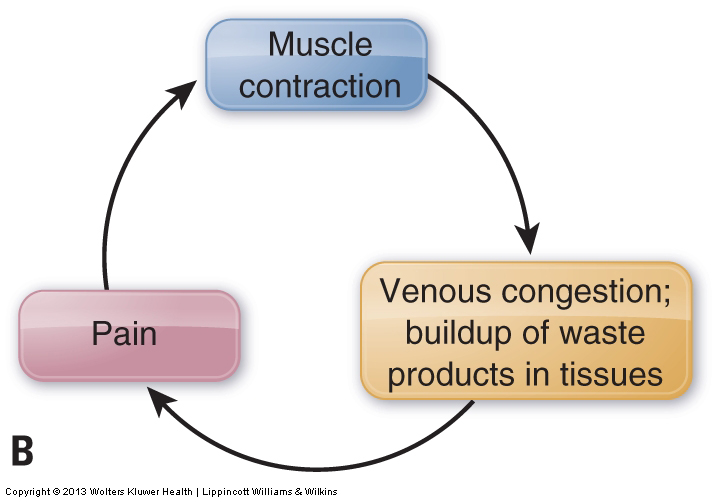
Overuse of a muscle fatigues it. Overuse also increases its level of tension. This increases the muscle’s pulling force on its tendons and bony attachments, irritating these structures and causing pain. In response to this pain, the nervous system signals the muscle to contract, which creates increased tightness of the entire muscle. This is a protective mechanism meant to decrease or prevent motion that might further irritate or injure the musculature and/or other soft tissues. Muscle tightness causing pain, which then triggers further tightness, which then triggers further pain, and so forth, is known as the pain-spasm-pain cycle. Prolonged contraction of a muscle can also result in a disruption of the blood circulation to the area. Initially, the prolonged contraction interrupts venous return of blood, causing a buildup of waste products. These waste products are acidic and irritate the muscle tissue, causing increased pain, which then further perpetuates the pain-spasm-pain cycle. The result is increased reflexive spasm of the muscle (Fig. 3).
Muscle overuse is often thought of in terms of an activity such as playing sports or working out at a gym. If the same muscle or muscle group is used repeatedly without rest, it will gradually fatigue and become painful. However, overuse can also result from prolonged unhealthy postures. Although less dramatic, poor posture is often a greater contributor to muscle tightness than overuse from activity. One of the most common postures that causes tightness of neck musculature is when the head is flexed forward such that its weight is no longer centered over the trunk. Examples would be working on a laptop computer or handheld electronic device that is placed too low in front, or reading a book held in the lap. Without muscles to counteract its motion, the head would naturally fall with gravity until the chin hits the chest. However, muscles in the posterior neck involved in extending the head and neck, such as the semispinalis capitis and the upper trapezius, prevent this by contracting isometrically to hold the imbalanced posture (Fig. 4A). Because of the tremendous amount of time that many people spend in postures that require the head and neck to incline into flexion, tightness of the posterior neck is much more common than anterior neck tightness.
Another example of overuse is carrying a bag or purse on the shoulder. To prevent the bag from sliding off, the body isometrically contracts the muscles that elevate that shoulder. In this case, muscles such as the upper trapezius and levator scapulae that attach to the scapula may be used/overused (Fig. 4B). Other examples of postural stresses range from working on a computer with the monitor set to the side, leaning over a desk when doing paperwork, or even talking to someone for a long time with the neck turned to the side. With excessive use, postural muscles of the neck will likely fatigue and tighten.


- Muscle Splinting
Muscles of the neck may tighten not only if the muscles themselves are irritated and overused, but also if any other tissues of the region become irritated or injured. This is especially true of the tissues of the neck joints, such as the ligaments and facet joint capsules. This phenomenon is called muscle splinting, and it is a protective mechanism for these fragile and vulnerable tissues. By tightening, the musculature acts as a splint to the area, blocking motion and thereby allowing the tissues of the area to rest and heal. Therefore, overt traumatic injury or irritation to any tissues of the neck can cause the muscles of the neck to tighten and splint the area.
- Adaptive Shortening
Adaptive shortening occurs when a muscle is held in a shortened state for a prolonged time and adapts to that shortened state by increasing its tone. Adaptive shortening is a protective mechanism. If a muscle is shortened and slackened, then when it contracts to create tension to move the body, the muscle would be unable to generate tension on its attachments until all the slack has been removed. This would not only cause an inefficient delay in movement, it could also be dangerous in a fight-or-flight scenario. For this reason, the nervous system adaptively shortens the muscle by increasing its tone to match the shortened length. The net result is that if a certain posture is held for a long time, the musculature will shorten and adapt to that posture so it is ready to create tension and movement immediately if needed. For example, if a lot of time is spent with the head and neck flexed, whether it is to work with a laptop computer, read a book, do paperwork at a desk, chop vegetables on a counter, or tend to an infant, the flexors in the front of the neck will adaptively shorten and become tight (locked short). Their tightness will then tend to perpetuate this posture, placing an increased strain/workload on the posterior extensor muscles (which become locked long).
- Muscle Overstretching
Another common reason for the neck muscles to tighten is overstretching of the musculature. As described previously, overstretching can activate the muscle spindle’s stretch reflex and cause a spasm if the neck is stretched too fast or too far. Even though this reflex is protective, the spasming often persists long after the initial event that triggered it, resulting in a chronic posture of tight musculature of the region.
Overstretching a muscle can be caused traumatically, as with a whiplash or other injury. It can also occur when doing stretches as part of a health and fitness regimen. This is especially true if stretching is done too vigorously when the muscles have not yet warmed up, as often occurs when stretching is done before an exercise routine. For this reason, it is increasingly recommended that stretching be done after exercising, when the muscle tissues are warm. Thus, even though stretching is a valuable part of a health and fitness regimen, when it is performed too aggressively, it can be detrimental to musculoskeletal health. Moderation is the key.
Overstretching also often occurs in a much more insidious and seemingly innocuous manner. Simple postures assumed and carried out during the day can be the culprit. Examples include poor ergonomics at the workplace, such as working in front of a computer monitor placed to the side instead of directly in front of the worker, or cradling/crimping a phone between a shoulder and ear for prolonged periods. These postures may also occur outside of work during daily activities, such as sitting with the neck rotated while talking to a friend, or flexing the neck downward to work with a smart phone, mp3 player, or other electronic devices. Sleep postures can be equally problematic, such as sleeping on the stomach with the neck rotated to one side. This posture can easily cause an overstretch of the rotators that are antagonistic to the direction of the neck’s rotation, resulting in waking during the night or the next morning with tight muscles caused by the stretch reflex.
MYOFASCIAL TRIGGER POINTS:
The other type of hypertonic musculature is a myofascial trigger point, often referred to simply as a trigger point (TrP), and known in lay terms as a muscle knot. As described previously, a TrP is a focal area of muscle tightness that can refer pain to a distant site. TrPs are often divided into active and latent TrPs. Latent TrPs require pressure to be applied to them for referral of pain to occur. Active TrPs can refer pain without pressure.
Mechanism of Myofascial Trigger Points
Unlike globally tight musculature, whose mechanism is the muscle spindle reflex under the direction of the gamma motor system of the brain, a myofascial TrP is a local phenomenon. Muscle contraction occurs via the sliding filament mechanism. During this mechanism, crossbridges of myosin and actin (filaments found within the muscle fibers) constantly form, release, and reform to create the muscle contraction. Necessary to the release of these crossbridges is supply of energy in the form of adenosine triphosphate (ATP) molecules, which are created by a supply of glucose (blood sugar) delivered in the arterial blood supply to the musculature. If this arterial blood supply is cut off (often due to compression caused by the muscle’s own contraction), then the muscle tissue is deprived of nutrients, including glucose. This loss of arterial blood supply is called ischemia; the creation of ischemia by muscular contraction is called the contraction-ischemia cycle (Fig. 5).
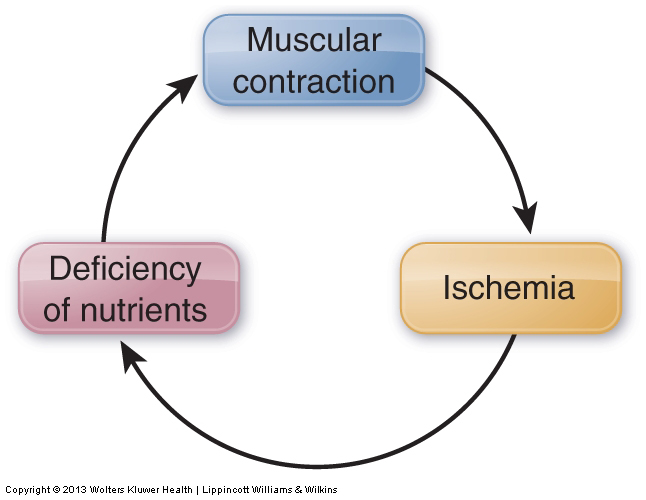
When ischemia, resulting in the loss of ATP formation, occurs in a small region of muscle fibers, the crossbridges in this region cannot be released and a TrP forms. Therefore, the mechanism for TrP formation and especially TrP perpetuation is ischemia at the local level. This phenomenon is usually referred to as the energy crisis hypothesis (because of the crisis of a lack of ATP, i.e., the energy source of the cell). Treatment should be aimed at relieving ischemia by manual and movement therapies that increase local blood circulation. Deep stroking massage (usually for a duration of approximately 30 to 60 seconds) is increasingly being recommended as the treatment of choice to work a myofascial TrP.
Causes of Myofascial Trigger Points
The four most common causes of myofascial TrPs are:
- Acute or chronic overuse of the muscle, including concentric contraction with activity as well as isometric contraction with posture
- Chronic stretch of the muscle
- Prolonged immobility of the muscle
- Trauma/injury to the muscle
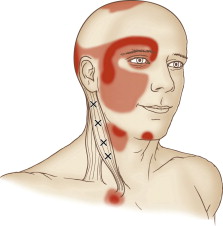
Common Myofascial Trigger Points of the Neck and Their Referral Zones
A TrP can form anywhere within a muscle. However, there are certain locations within muscles where TrPs tend to form more commonly than others. Further, each TrP within a muscle tends to have a characteristic referral zone. Each referral zone is usually divided into a primary and secondary referral zones. A TrP most commonly refers to its primary referral zone; when more severe, it usually also refers to its secondary referral zone. Figure 6 illustrates a muscle with common TrP locations and their corresponding referral zones. The locations of TrPs are indicated by Xs. Primary referral zones are indicated in dark red; secondary referral zones are indicated in light red (Fig. 6).
Figure 6. Figure Courtesy of Joseph E. Muscolino. The Muscle and Bone Palpation Manual with Trigger Points, Referral Patterns, and Stretching. 2ed. Elsevier. 2016
Summary of Hypertonic Musculature
It is important to distinguish between globally tight musculature and myofascial TrPs because optimal treatment approaches differ for the two conditions. Manual and movement therapy for a globally tight muscle might be performed locally at the tight muscle, but its intended consequence is to cause the gamma motor system of the central nervous system to change its pattern of muscle memory that determines the tone of that muscle. In contrast, treatment of a TrP is primarily aimed directly at causing a local change in the muscle tissue itself, increasing blood supply where the TrP is located.
However, all hypertonic musculature, whether it is a globally tight muscle or a myofascial TrP, can decrease motion at the joint that is crossed by that muscle. Once joint motion has been restricted for a prolonged time, the functioning of that joint may become impaired. This condition is known as joint dysfunction and is discussed in the following blog post article in this series.
Brief Overview of Treatment Considerations For Hypertonic Musculature
Therapeutic manual therapy for spasmed muscles of the neck follow from a thorough and accurate assessment/diagnosis. So a proper assessment of neck musculature should be performed. Most every manual and movement therapy technique addresses tight musculature. Manual therapy for spasmed muscles of the neck can be especially beneficial. Certainly all forms of massage therapy, stretching, and hydrotherapy are effective for the treatment of hypertonic musculature and fascial adhesions. In particular, deep stroking massage is recommended for the treatment of myofascial TrPs. And pin and stretch technique is effective when trying to focus the stretch force to a region of a muscle. Movement therapy also addresses lengthening myofascial tissues, which can decrease tight musculature and help to break up fascial adhesions. Given that tight muscles are usually accompanied by hypomobile joint dysfunction, joint mobilization is often a necessary adjunct to manual therapy treatment for the client with hypertonic (tight) neck musculature.
As a general rule, with any manual therapy treatment to the neck, there are always precautions and contraindications to consider given the number of sensitive structures present.
(Click here for a blog post article on manual therapy treatment for clients with spasmed muscles of the low back.)
(Click here for a blog post article on hypertonic tight muscles of the low back and pelvis.)
Note: This blog post article is the second in a series of 10 posts on
Common Musculoskeletal* Conditions of the Neck
The 10 Blog Posts in this Series are:
- Fascial Adhesions (and an introduction to musculoskeletal conditions of the neck)
- Hypertonic (tight) musculature
- Joint dysfunction
- Sprains and strains
- Pathologic disc conditions
- Osteoarthritis (OA)
- Thoracic outlet syndrome (TOS)
- Forward head posture
- Tension headaches
- Greater occipital neuralgia
(*perhaps a better term is “neuro-myo-fascio-skeletal”)


