Signs and symptoms of plantar fasciitis:
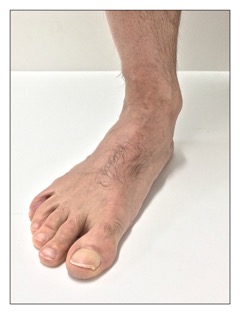
A collapsed arch structure (overpronation) of the foot on weight bearing. Permission: Joseph E. Muscolino.
The most common symptom of plantar fasciitis is pain on the plantar side of the foot, most often located near the calcaneal attachment. Pain is usually worst first thing in the morning. Pain also increases with weight bearing (standing, walking, or running), although some walking can actually help decrease symptoms because it helps to loosen the plantar soft tissues. Pressure against the plantar fascia also increases the pain. This can occur if the client/patient wears a shoe with a hard or excessively high arch. As the name of this condition implies, inflammation is also present (“itis” means inflammation). It can occur along the entire length of the plantar fascia, but is usually worst at the calcaneal attachment. Ironically, even though this condition is usually caused by pulling (tensile) forces placed upon the plantar fascia, because of the irritation and swelling that occur, the plantar fascia usually becomes taut. This is due to tightening of the intrinsic plantar musculature that tightens in response to the stretching, irritation and pain, as well as fascial adhesions in the plantar fascia that form over time.
With chronic cases of plantar fascia, as with other pathologic conditions of fibrous fascia, the swelling often recedes and is replaced with degeneration of the collagen matrix of the fascia. This is similar to the transition of tendinitis to tendinosus in tennis or golfer’s elbow.
Assessment/Diagnosis of plantar fasciitis:
Assessment/diagnosis of plantar fascia is straightforward. Pain is reported by the client/patient at the underside of the foot, and can be palpated at the plantar fascia, especially at or near the calcaneal attachment. Inflammation is usually not readily palpable because of the thickness of the subcutaneous tissues, but may be detected in more severe cases. If inflammation is not palpable, it might also be due to a transition from an inflammatory condition to one of collagen degeneration (in effect, fasciitis transitional to “fasciosis”); this often occurs with chronic cases.
Stretching the plantar fascia by extending the toes at the metatarsophalangeal joints and pronating the foot (moving it into dorsiflexion, eversion, and lateral rotation/abduction) also likely increases the characteristic pain of the condition. The tautness/tightness of the plantar fascia is usually palpable.
It is important to also assess for tightness of, or myofascial trigger points in, the plantar intrinsic musculature, especially those that attach into the plantar fascia (the abductor hallucis on the big toe side, the abductor digiti minimi pedis on the little toe side, and the flexor digitorum brevis located between the other two). These muscles are usually tight in the client/patient who has plantar fasciitis, whether it is in response to the pain or in an attempt to prevent excessive stretching of the plantar fascia during the pronation phase (heel strike to midstance) of the gait cycle.
Postural examination likely reveals overpronation of the foot upon weight bearing: standing, marching in place, or walking. Observation can be done from the anterior or the posterior view: anteriorly, observe the medial longitudinal arch itself; posteriorly, look for a bend in the Achilles tendon. Another way to check for overpronation is to observe the client’s/patient’s leg (tibia) and thigh (femur) when weight bearing; with overpronation, the tibia and femur will be seen to fall into medial rotation when the client/patient weight bears. This can usually be best seen by observing the posture of the patella. If overpronation is found, then it is important to assess for the many factors that can cause overpronation.
Differential assessment of plantar fasciitis:
Local pain directly over the calcaneal tuberosity at the underside of the calcaneus is typical with plantar fasciitis; it is also typical when the client/patient has a heel spur. Because the presence of a heel spur is usually caused by tight/taut plantar fascia or plantar fasciitis, these two conditions usually occur together. Indeed, it is rare for a heel spur to occur in a client/patient who has healthy plantar fascia. Therefore, the presence of a heel spur can be viewed as further confirmation of plantar fasciitis.
Pain on the underside of the foot can also be caused by tightness of and/or myofascial trigger points in the intrinsic plantar musculature of the foot. Tightness in this musculature often accompanies plantar fasciitis, but may occur on its own. Plantar foot pain can also be caused by stress fractures of the metatarsals, Morton’s neuroma, or tendon dysfunction of extrinsic muscles of the leg that attach into the foot (often the tibialis posterior).