Self-care for the client/patient with shin splints
Self-care for shin splints begins with RICE: rest, ice, compression, and elevation. If the client/patient has anterior shin splints that is caused by running or some other physical activity that involves running, the client/patient should stop the activity until the condition is resolved. If the condition is not severe, then the client/patient might be able to continue participating in the sport if either the distance that is being run is decreased or the client switches to running on a softer surface. However, it is also likely that continuing to run will delay healing and prolong the condition. If the client has posterior shin splints that is caused by an activity that involves plantarflexion, the client should stop or lessen this activity.
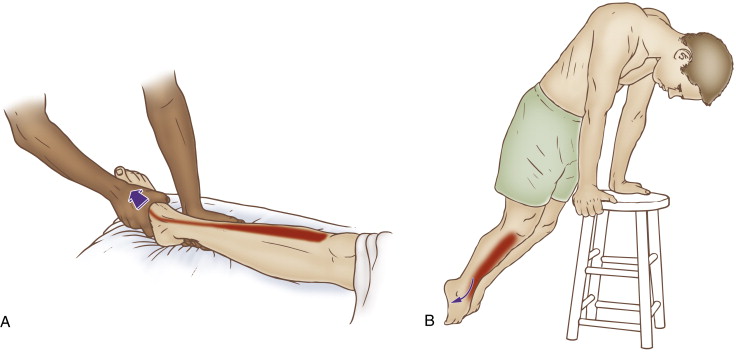
Self-care (and therapist assisted) stretch for the tibialis anterior. Permission: Joseph E. Muscolino. The Muscle and Bone Palpation Manual – with Trigger Points, Referral Patterns, and Stretching, 2ed (Elsevier, 2016).
A good guideline for icing is to apply ice to the affected region until the area is numb; icing should be done a minimum of two to three times per day until the condition is resolved and the pain is gone. Compression to the region can be done by wearing a compression sleeve made of neoprene or some other material like nylon and spandex. If overpronation is one of the causative factors, consider recommending to the client/patient to either get orthotics or shoes that have good arch support.
Once the acute phase of shin splints is over, strengthening the involved musculature can be helpful. Individual muscle groups can be easily exercised at home with resistance tubing. Plantarflexion musculature (e.g., the soleus) can be easily exercised with heel raises. The client/patient simply stands and then rises up on their heels (engaging the muscles of plantarflexion concentrically) and then slowly lowers their body back down (engaging the muscles of plantarflexion eccentrically). The client/patient should do one set of heel raises until the musculature reaches exhaustion, working up to the goal of performing a set of 100. One to three sets should be done per day.
Medical approach to shin splints
The medical approach to treatment of shin splints is usually RICE and the addition of anti-inflammatory medication, whether it is a non-steroidal anti-inflammatory drug (NSAID) or cortisone/prednisone (steroidal anti-inflammatory drug) medication.
Manual therapy case study for shin splints
Rolando is a 16-year-old boy who runs distance events for his high school track team. Several weeks ago, he increased the mileage he was running and began to notice pain in the front of his (lower) leg. He went to a massage therapist who was doing post event massage at one of his track meets.
The therapist noted mild swelling along the tibialis anterior attachment at the lateral border of the tibia; palpation to the attachment was tender and painful. The tibialis anterior was moderately tight and contained myofascial trigger points. Manual resistance to dorsiflexion and inversion of the foot was mildly painful and reproduced the characteristic pain that Rolando has been feeling. Stretching the foot into plantarflexion and eversion also produced mild anterior leg pain. The extensors digitorum and hallucis longus were also mildly tight and tender to palpation. The therapist told Rolando that it was likely that he had a mild case of anterior shin splints and recommended RICE and massage therapy.
Rolando followed the therapist’s recommendations and iced his leg two to three times every day. He also bought and used a neoprene compression sleeve for his right leg. Because the severity of the shin splints was not bad, he decided to continue running with the track team but eased up on his workouts, running fewer miles, and when possible running on the grass on the interior of the track to avoid the harder surface of the track. He temporarily dropped out of competing at track meets.
He also began having clinical orthopedic massage from the massage therapist who he had met at his track meet. The massage therapist began by working the musculature of the anterior leg, with emphasis on the tibialis anterior. Longitudinal strokes with mild to moderate pressure were performed followed by cross-fiber strokes. Only light effleurage was done at the actual tibial attachment of the tibialis anterior, from distal to proximal in direction. Heat was applied to the anterior compartment musculature with the leg elevated. Deep short stroking was then performed on the myofascial trigger points and the tibialis anterior was stretched into plantarflexion and eversion. Ice was then applied to the anterior and lateral border of the tibia while the therapist performed soft tissue manipulation to the rest of Rolando’s lower extremities. The therapist mobilized (arthrofascially stretched) Rolando’s tarsals and metatarsals; and then spent the remainder of the hour working on Rolando’s back and upper extremities. This treatment was repeated once each week for another two weeks.
At the end of three weeks, Rolando’s condition was resolved and he was able to gradually increase his workouts with the track team, this time slowly increasing his mileage to allow his musculature time to strengthen and accommodate the increased physical stress of the workouts. Rolando has decided to continue seeing the massage therapist for proactive care approximately 1-2 times per month.


