Self-care for the client/patient with plantar fasciitis:
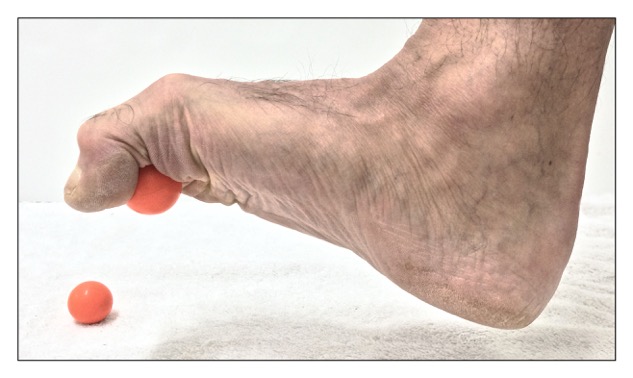
Self-care strengthening exercise for the intrinsic musculature of the foot for a client with plantar fasciitis. Permission: Joseph E. Muscolino.
As with any inflammatory condition, self-care for plantar fasciitis begins with RICE: rest, ice, compression, and elevation. Most important of these are ice and rest; it is important that the client/patient decrease weight-bearing activities. As appropriate, the client/patient can be instructed to perform gentle self-massage and stretching to the underside of the foot. Foam rolling or rolling on a ball can also be very effective. If overpronation is present, then it should be addressed; in the short term, supportive and comfortable shoes and arch supports can be recommended. For the long term, the underlying cause of the overpronation (collapsed arch structure) must be addressed.
Medical approach to plantar fasciitis:
The medical approach to treatment of plantar fasciitis is usually RICE and the addition of anti-inflammatory medication, whether it is a non-steroidal anti-inflammatory drug (NSAID) or cortisone (steroidal anti-inflammatory drug) medication. It is likely that X-Rays will be ordered to rule out a stress fracture in the foot. Platelet rich plasma (PRP) injections can also be done for any fascial tissue degeneration.
Manual therapy case study for plantar fasciitis:
Clare is a 41-year-old artist who began to have pain on the plantar side of her left foot a few months ago. At first, her pain was present only when she jogged or spent prolonged periods of time standing at the easel. But after a couple of months, she noticed that the foot pain would begin sooner when jogging or working at the easel, as well as other times during the day when she ran errands. She went to her medical doctor who ordered an X-Ray and told her that she has a heel spur, and stated that it was cause of her pain. He recommended that she stay off her feet and take over the counter anti-inflammatory medication as needed. A month later, her pain was only mildly reduced, so she decided to try seeing a massage therapist whom she was told has worked with this type of orthopedic problem.
The therapist palpated her foot and found that her plantar fascia was extremely tight and painful. The pain was especially acute at the calcaneal attachment. Stretching the plantar fascia also increased her pain. Mild swelling was also present along the plantar fascia, most markedly near the calcaneal attachment. And myofascial trigger points were found in the intrinsic musculature of her foot. Postural exam revealed that Clare markedly overpronates her left foot upon weight bearing.
The therapist told Clare that the cause of her pain is more likely the plantar fasciitis and that the underlying cause is overpronation. The therapist agreed with the medical doctor that rest and anti-inflammatory medication would be helpful. But the therapist told Clare that her foot pain would probably not go away unless the plantar fascia was treated, and more importantly, the overpronation was corrected. The therapist told her she could passively correct the overpronation with orthotics, but that to truly correct the overpronation, active exercises would be needed. Due to the acuteness of the plantar fasciitis, Clare decided to buy orthotics immediately to correct her overpronation and found a pair that was supportive but soft enough so as to not irritate the plantar fascia. The therapist further recommended that Clare use a foam roller on the underside of her foot.
For treatment, the therapist began with mild to moderate pressure soft tissue manipulation to the entire right thigh and leg, especially the tissues of the superficial posterior myofascial meridian, gradually working her way distally to Clare’s foot. On the plantar side of the foot, she performed gentle long strokes from heel to toe along the plantar fascia, and then transversely across the plantar fascia. As myofascial trigger points were encountered in the plantar musculature, the therapist increased the pressure and performed deep stroking massage across them. She then performed gentle stretching of the foot and finished working Clare’s foot with joint mobilization (arthrofascial stretching). To decrease the likelihood that the treatment would cause increased swelling, the therapist iced Clare’s foot at the end of the session. With whatever time was left over, the therapist worked Clare’s pelvis, low back, and her other lower extremity. This protocol was performed twice a week for five weeks.
The therapist also recommended that Clare begin strengthening the intrinsic musculature of her foot with a simple self-care strengthening exercise. Clare was instructed to pick up small balls or marbles with her toes.
At the end of five weeks, Clare’s condition was nearly entirely resolved and she was able to stand comfortably for longer periods of time. She decided to replace jogging with a Pilates apparatus workout to strengthen her arches as well as her entire body. Clare also decided to continue seeing the massage therapist for proactive care approximately once a month.