The Major (“True”) Function of the Gluteus Medius
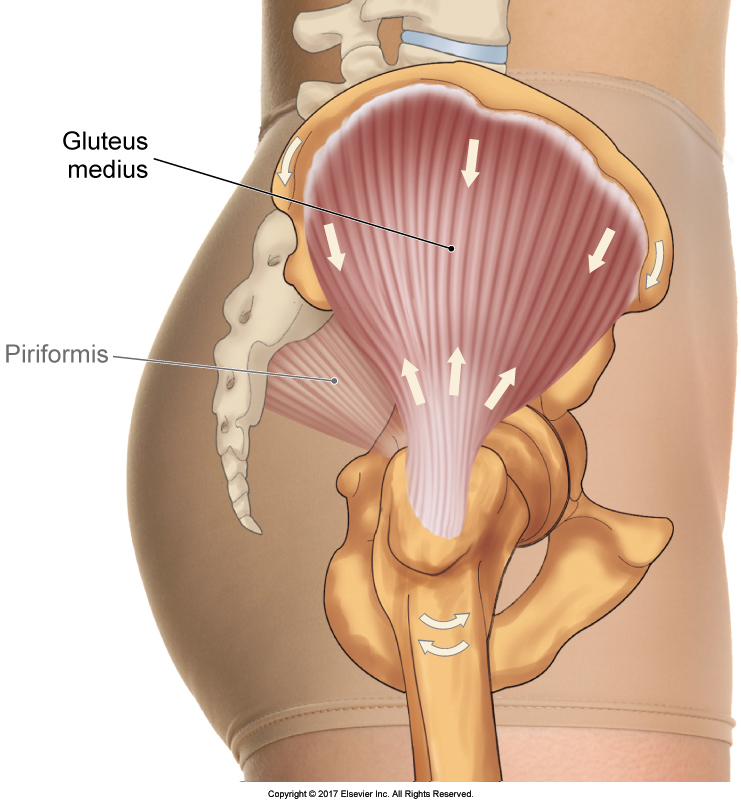 The gluteus medius (Figure 1) is a muscle that all students and therapists are aware of; we all learn it. If you ask someone what the function of this muscle is, most likely you will be told that it abducts the thigh at the hip joint. Even though this is an action of the muscle and the one that most everyone learns in school, it is not its most important function. After all, how often in life do we really need to lift our thigh out to the side of our body? This may be what is taught in school and written in most books, but it does not reflect its major (“true”) function in everyday life.
The gluteus medius (Figure 1) is a muscle that all students and therapists are aware of; we all learn it. If you ask someone what the function of this muscle is, most likely you will be told that it abducts the thigh at the hip joint. Even though this is an action of the muscle and the one that most everyone learns in school, it is not its most important function. After all, how often in life do we really need to lift our thigh out to the side of our body? This may be what is taught in school and written in most books, but it does not reflect its major (“true”) function in everyday life.
Figure 1. Lateral view of the right gluteus medius. Permission Joseph E. Muscolino. The Muscular System Manual – The Skeletal Muscles of the Human Body, 4th ed. Elsevier, 2017.
The major function of this muscle is its ‘reverse action’ (closed-chain action) when the thigh is fixed and it pulls on the pelvis (Figure 2B), not its usually thought of “standard action” (open-chain action) when the pelvis is fixed and it pulls on the thigh (Figure 2A)!
This occurs most often during the gait cycle (walking). When standing, our weight is balanced over our two feet. However, when we walk and take a step by lifting one foot up, our body weight is no longer balanced and instead is unsupported in thin air. This should cause our pelvis to fall to that (’swing-limb’) side. It is the role of the gluteus medius on the opposite support-limb side of the body to prevent this.
When the foot is on the ground (described as a closed-chain position), the thigh is not free to move. Therefore, when the gluteus medius contracts, the force of its pull is exerted on the pelvis instead, pulling it in the downward direction, known as depression or lateral tilt to that side. If one side of the pelvis is pulled down, the other side is elevated (also known as “hiking the hip”). The major function of the gluteus medius is to stabilize the pelvis with this downward direction of pull.
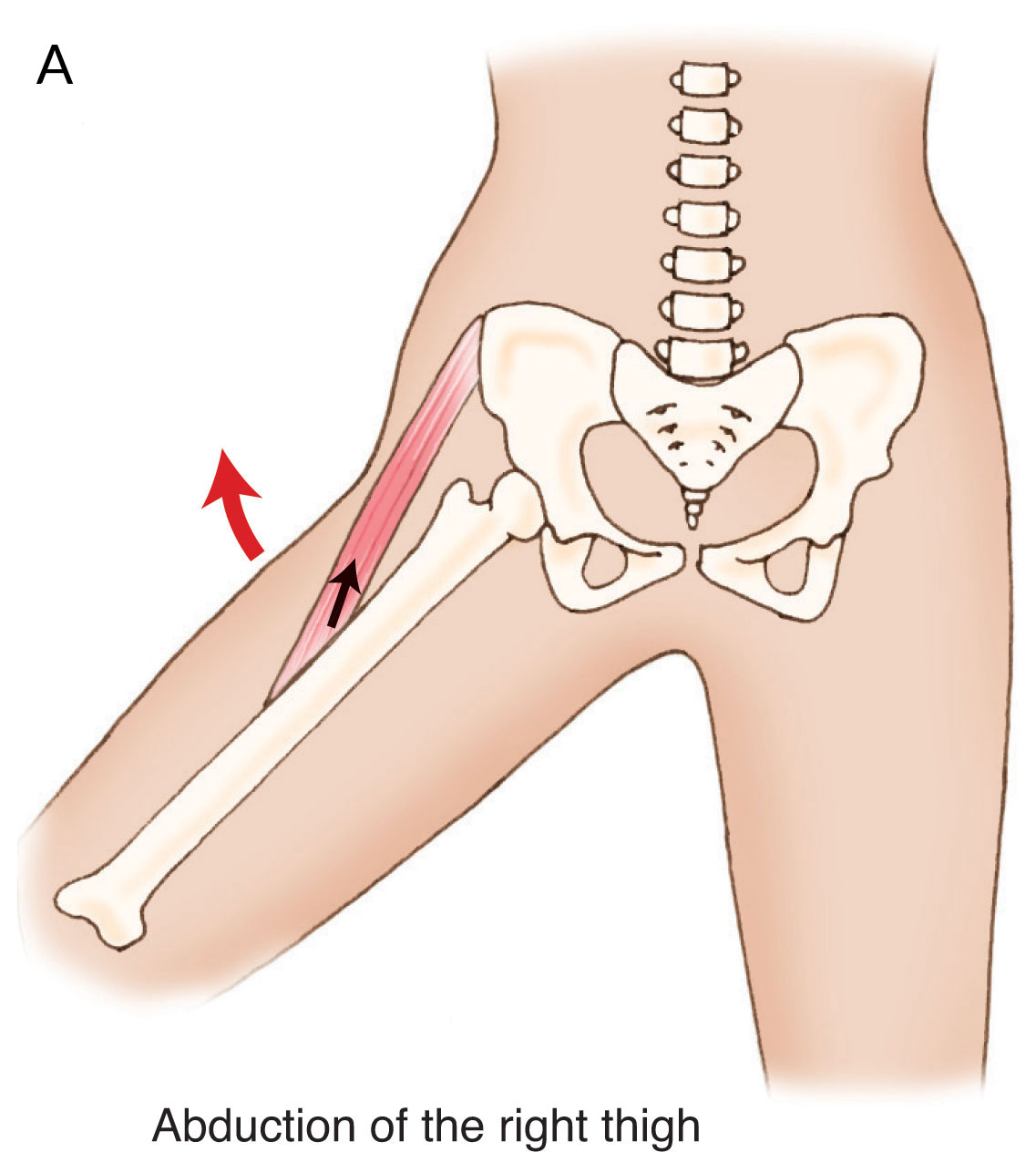
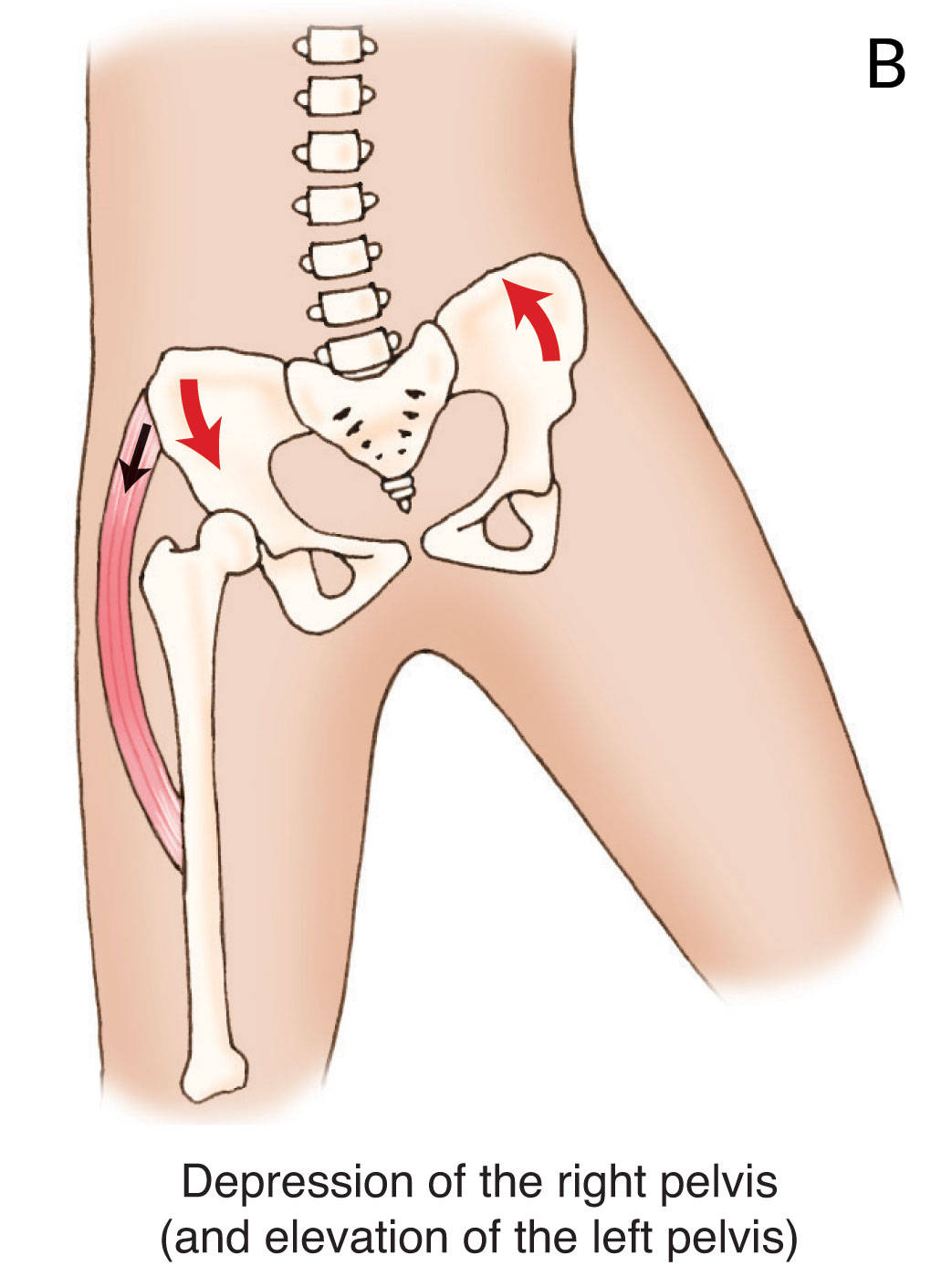
Figure 2. Joints actions of the gluteus medius. A, Standard open-chain action of abduction of the thigh at the hip joint. B, Reverse closed-chain action of depression of the pelvis at the hip joint. Permission Joseph E. Muscolino. Kinesiology – The Skeletal System and Muscle Function, 3ed. Elsevier, 2017.
For example, if I lift my right foot to take a step, my pelvis should fall to the right side. My left-sided (support-limb) gluteus medius prevents this by isometrically contracting and pulling downward on the left side of the pelvis, thereby preventing the pelvis from falling to the right. This is the major/true function of the gluteus medius! Every time we take a step, the gluteus medius on the ’support-limb’ side contracts to stabilize the pelvis. You can easily test this by standing up and palpating the gluteus medius on both sides by palpating immediately distal to the midpoint of the iliac crest on each side. Then slowly walk in place by lifting one foot at a time. You will feel the gluteus medius contract on the support-limb side every time! (In fact, as discussed later in this blog post aticle, you do not even have to actually lift a foot off the floor; you can experience the same activation of the gluteus medius by simply shifting your weight from foot to foot.)
Tip for students: Always look for the reverse action of a muscle. It is often its most important action, even if you did not learn it in school!
Tip for teachers: Teach the reverse (closed-chain) actions of muscles, especially those that attach to the pelvis. The pelvis is incredibly important toward spinal posture and motion. Further, give real life examples of when muscles function!
Tip for therapists: Always look for how the postures and activities of a person can lead to overuse and injury. Evaluate the client both posturally (statically) and when dynamically moving too!
- For more on this role of the gluteus medius, see Kinesiology – The Skeletal System and Muscle Function, 3ed. (Elsevier, 2017).
- For more on the gluteus medius itself, see The Muscular System Manual, The Skeletal Muscles of the Human Body, 4ed. (Elsevier, 2017).
What Might Cause a Tight Gluteus Medius?
We have now spoken about the major/true function of the gluteus medius being depression (lateral tilt) of the pelvis at the hip joint, not abduction of the thigh at the hip joint. A tip was given to therapists to consider a client’s static postures and dynamic motion patterns when evaluating why that client has a tight gluteus medius. After all, if we can determine what s/he is doing to create the problem, then perhaps we can prevent it from occurring in the first place, or at least eliminate a perpetuating factor.
SO.. what is one common and simple postural habit that would tend to lead to a tight gluteus medius…? The habit of standing with all or more of one’s weight on one leg! This will cause the gluteus medius on that side to tighten. Why? We have said that if you palpate the gluteus medius bilaterally while walking in place, you would feel the contraction of the gluteus medius on the ’support-limb’ side each time the other foot lifted off the ground (it contracts to stabilize the pelvis). Redo this palpation exercise, but this time, do not even lift your foot off the ground. Instead, just shift your weight from one side to the other. You will feel the support-side gluteus medius contract just by shifting your weight to that side! This means that when someone posturally stands with more weight shifted to that side, that side gluteus medius will have to isometrically contract to stabilize the pelvis far more than the other side gluteus medius has to; especially in someone who stands in this asymmetrical posture for many hours each day! This will likely lead to a tighter gluteus medius on that side, or at least myofascial trigger points on that side.
Note: Many sources state that the gluteus medius is rarely overly facilitated, rather it is more often overly inhibited. However, even weakened overly inhibited muscles often develop taut bands of musculature and myofascial trigger points that can lead to pain and dysfunction for the client. For this reason, whether a muscle is overly facilitated locked short or overly inhibited locked long, it should be addressed with manual and movement therapy!
Asking questions like this in your history can help you find these things out. Also, observing your clients’ postures when they are not aware that you are watching them will help too. Keep in mind that when you do a ‘formal’ postural exam with a client, they are very often self conscious about their posture and do not show you their true patterns. Good information to apply clinically!
The Postural Effect of a Tight Gluteus Medius
We have discussed what the major/true function of the gluteus medius is: creating an isometric stabilization force of depression of the pelvis at the hip joint. We also discussed that people who tend to stand and put more weight on one leg than the other predispose themselves to having a tight and dysfunctional gluteus medius.
Now let’s look at what the postural effect of having a tight gluteus medius is. Whenever a muscle contracts, it creates a pulling force toward its center. This pulling force is exerted equally at both attachments. Which one moves is based upon which one is more mobile, in other words, less fixed/stabilized. We usually think of the distal attachment of a muscle doing the moving. However, the proximal attachment can move too! When this occurs, it is called a reverse action. Reverse actions occur very frequently in the lower extremity because the foot is so often fixed on the ground, placing the lower extremity into closed-chain posture, making the distal attachment more fixed/stabilized than the proximal attachment.
So, when the gluteus medius is tight (overly facilitated) and we are lying down, it stands to reason that the femur is more likely to move than the pelvis because it is free to move (open chain scenario here). If we assess the client in this scenario, we may see the femur slightly abducted, in other words, slightly “lifted up and out” toward the outside. Looking at the relative alignment of the feet, that side foot may seem a bit higher and many therapists would describe it as being a “short leg” (i.e., “short limb”).
BUT, if we are standing up, the foot is fixed on the ground (closed chain) and will not easily move. So the pull of the gluteus medius acts upon the pelvis and can cause it to depress. If we are assessing the client’s posture in this scenario, we will likely see the iliac crest a bit lower on that side and again, may describe the client as having a short limb on that side.
Result: A tight gluteus medius can affect the posture of the client and create what is known as a “short leg/limb.” Because this short leg is the result of myofascial pulls, it is often described as a “functional short leg” (as opposed to a “structural short leg” caused by an actual length difference between the femur or tibia on one side compared to the other side).
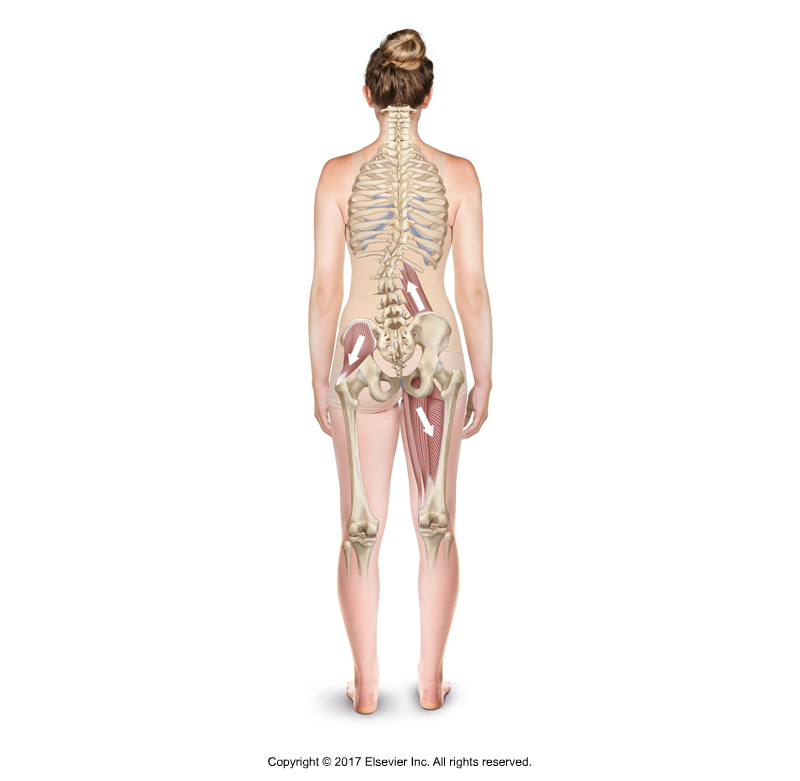
Many muscles can exert their pulls on the pelvis resulting in asymmetrical postural dysfunction patterns, such as a “short leg.”
Figure 3. A tight (overly facilitated) gluteus medius can cause a “short leg” on that side. Permission Joseph E. Muscolino. Kinesiology – The Skeletal System and Muscle Function, 3ed. (Elsevier, 2017).
Tip for Therapists: Working backward with this knowledge, when you find a client with a short limb, it is worthwhile to assess the gluteus medius on that side. Do this assessment when the client is relaxed and lying down.
Tip for students: Learning these muscles well in your science classes will make you a better clinical orthopedic manual (COMT) therapist!
Tip for Instructors: These real life postural examples make learning more interesting. You can apply this knowledge kinesthetically in class if you have the time. Have students check each other standing postures, looking for a short limb. Then have them lie down and assess to see if the gluteus medius is more often tight on the short side than the ‘long’ side.
- For more on the gluteus medius and its role in posture, and posture in general, see Kinesiology – The Skeletal System and Muscle Function, 3ed. (Elsevier, 2017).
Of course, let’s always keep in mind that there are other factors that can create a short limb. The gluteus medius is only one piece of the puzzle.
Note: Something to think about: Could a tight gluteus medius also pull the pelvis down into depression when the client is lying down? Would the pelvis be sufficiently mobile in that position?
Treating the Gluteus Medius with Manual Therapy
Now that we have addressed understanding the function and postural effect of the gluteus medius, let’s look at treating it with manual therapy soft tissue manipulation and stretching.
What are our goals when treating myofascial tissue? In general, we have two major aims:
- to reduce muscular hypertonicity (i.e., contractile tone)
- to reduce fascial adhesions.
With respect to soft tissue manipulation (massage), keep in mind that the posterior fibers of the gluteus medius are deep to the gluteus maximus and the anterior fibers are deep to the tensor fasciae latae (TFL); the middle fibers are superficial but are deep to a fairly thick layer of fibrous fascia. Cross fiber techniques coupled with some long stripping strokes from proximal to distal work very nicely. Working it on stretch can be effective for the middle fibers but is usually not as effective for the deeper anterior and posterior fibers (working myofascial tissue on stretch is usually more effective for superficial myofascial tissue). And pin and stretch technique is an extremely effective way to focus the force of the stretch to a specific region of the gluteus medius.

Figure 4. Stretching the gluteus medius (and all hip abduction musculature) in side-lying position. Note the stabilization of the pelvis to prevent it from depressing. Permission Joseph E. Muscolino. Manual Therapy for the Low Back and Pelvis – A Clinical Orthopedic Approach. 2015.
Stretching is extremely effective for the gluteus medius and should be done after it has been warmed up with massage and/or heat (Figure 4). The combination of heat, massage, and stretching is an extremely 1, 2, 3 punch routine that is my go-to “default guideline” for effective clinical orthopedic manual therapy for tight/taut myofascial tissue. Of course, the treatment strategy that we finally decide on should depend on the specific circumstance of each client and how they respond to the care that we give.
We never want to treat with cookbook recipes, rather we want to match the mechanisms of our treatment approaches with the mechanisms / pathomechanics with which the client presents!
Critically think… Creatively apply!
Note: For further information on continuing eduction (CE) for Certification in Clinical Orthopedic Manual Therapy, click here.


